Respite Grants and Vouchers: Where to Apply and How to Qualify for Family Caregiver Financial Assistance
Caring for a loved one often creates both emotional strain and practical financial pressure, and respite grants and caregiver vouchers are two practical tools designed to ease that burden. This article explains what respite grants and caregiver vouchers are, summarizes typical eligibility rules, and shows where and how family caregivers can apply for payment programs including Medicaid HCBS waivers, VA supports, and state respite offerings. Readers will learn the core distinctions between grant-, voucher-, and waiver-based payment models, step-by-step application guidance with a documents checklist, and state-specific direction for Indiana, Michigan, and Illinois. The guide also outlines common roadblocks and gives clear next steps so caregivers can plan applications, gather evidence, and pursue timely approvals.
What Are Respite Grants and Caregiver Vouchers? Definitions and Benefits Explained
Respite grants and caregiver vouchers are government- or nonprofit-funded programs that pay for short-term relief or subsidize paid care so family caregivers can take a temporary break or be compensated for their time. These programs work by allocating funds to eligible care recipients or caregivers, enabling purchase of respite services, hiring of a paid caregiver, or issuance of vouchers that cover a defined set of services. The primary benefit is twofold: immediate relief from caregiving duties and a financial resource that compensates family caregivers for time spent providing in-home care. Understanding these program mechanics clarifies who should apply, what documentation is needed, and how to plan for reoccurring or one-time respite periods.
What is a respite grant and how does it provide financial relief?
A respite grant is a funding award—often from state, federal, or nonprofit sources—earmarked to pay for temporary caregiver relief, such as in-home respite visits, adult day services, or short-term institutional stays. Grants typically prioritize care recipients with demonstrated functional needs or family caregivers facing documented stress or burnout, and awards may cover a defined number of hours or a capped amount over a set period. For example, a family might use a respite grant to fund several days of in-home help while arranging longer-term care plans, which reduces immediate risk of caregiver fatigue and emergency hospitalization for the care recipient. Knowing the typical funders and allowable uses helps caregivers target programs that match their situation and timing.
How do caregiver vouchers work to support family caregivers?
Caregiver vouchers function like a prepaid benefit: an eligible care recipient or caregiver is issued a voucher or credit that can be redeemed for approved services, a selected agency, or an independent provider, including—where permitted—qualified family members. Vouchers outline allowable services, maximum hourly or daily limits, and redemption procedures and often require enrollment and verification before payments are made. Restrictions vary: vouchers may be time-limited, restricted to licensed providers or to non-family providers, or allow self-direction where the caregiver is paid directly. Understanding voucher rules helps families choose between using vouchers for short-term relief or as part of a longer-term consumer-directed care arrangement.
What Are the Eligibility Requirements for Respite Care Grants and Vouchers?
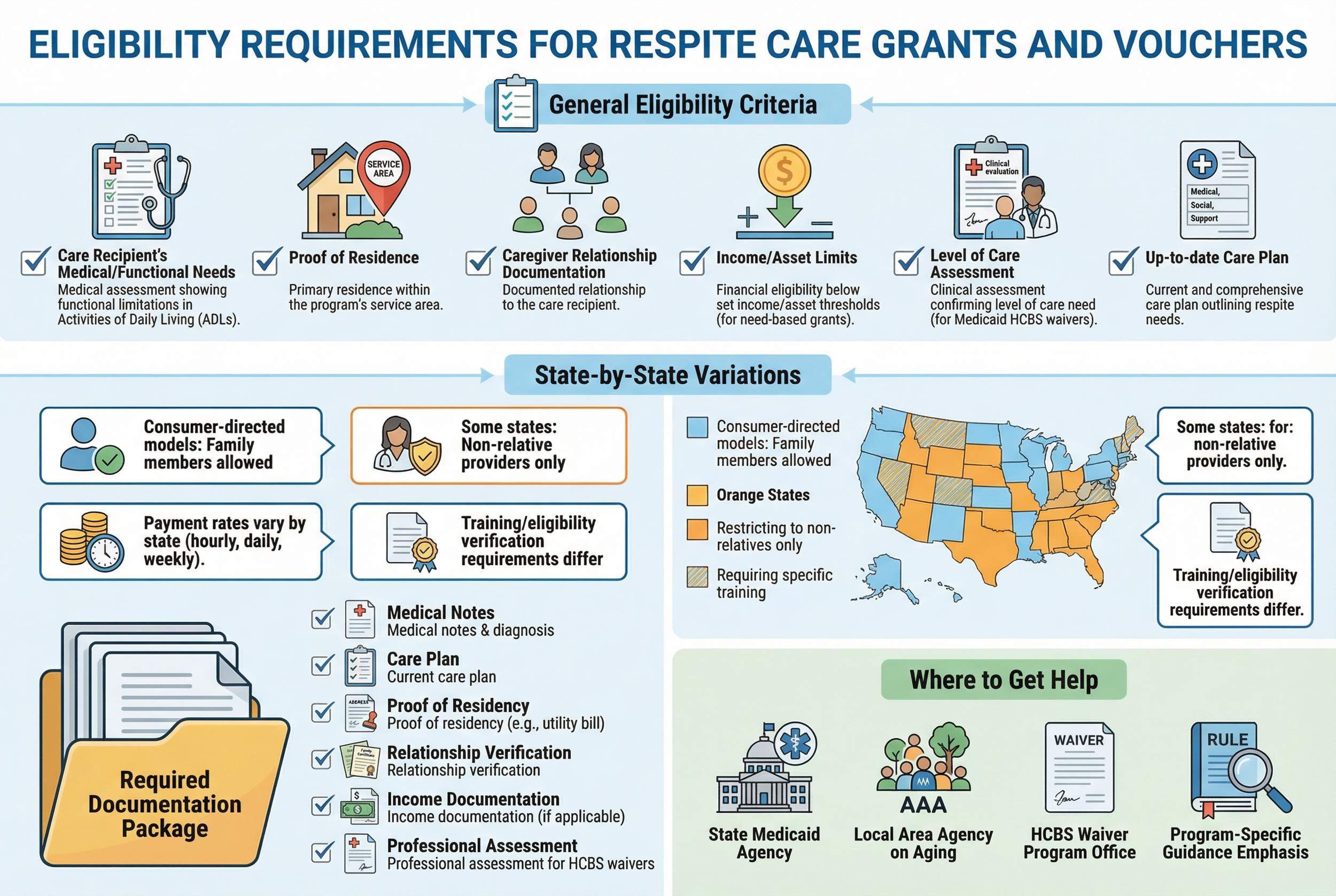
Eligibility for respite grants and caregiver vouchers centers on the care recipient’s needs, residency, and sometimes household income; states and programs then add their specific rules and documentation requirements. Most programs require evidence of a qualifying condition or a functional need—such as limitations in activities of daily living—and residency in the program’s service area. Some grants are need-based and include income or asset limits, while many voucher and waiver programs emphasize level-of-care and clinical assessments rather than strict financial eligibility. Clear documentation and an up-to-date care plan speed approvals and reduce requests for follow-up evidence.
What general criteria determine eligibility for caregiver financial assistance?
Most caregiver-support programs apply a consistent set of eligibility criteria that determine whether an application will move forward to assessment and potential approval. Common criteria include the care recipient’s medical or functional needs, proof of residence within the issuing jurisdiction, documentation of the caregiver relationship or household status, and, where applicable, income or asset limits tied to means-tested grants. Programs that rely on Medicaid HCBS waivers emphasize clinical level-of-care and often require a professional assessment and care plan that justifies home- or community-based services. Preparing a clear packet with medical notes, a care plan, and proof of residency addresses the most frequent reasons applications stall.
How do eligibility requirements vary by state for Medicaid waivers and respite programs?
States design waiver and respite programs differently, producing variation in allowable paid caregiver relationships, rate-setting, and program caps. For example, some states explicitly allow hiring family members under consumer-directed models, while others restrict payments to non-relative providers or require specific training or eligibility verification for family caregivers. Payment rates and frequency (hourly, daily, weekly) are state-determined and can affect whether a caregiver opts for a voucher, waiver, or public grant. To navigate these differences, caregivers should consult their state Medicaid agency and local Area Agency on Aging for program-specific rules and to learn whether family caregivers can be paid directly.
Which Government Programs Pay Family Caregivers? Overview of Key Funding Sources
Multiple program categories can fund caregiver payments, with Medicaid HCBS waivers often providing the most direct path to paying family members through self-directed models, while other sources like VA benefits, state respite grants, and paid family leave offer complementary routes. Understanding each funding source’s payer, covered services, and typical payment structure helps caregivers choose the right application pathway. Programs differ on whether they cover personal care, skilled nursing tasks, respite hours, or wage replacement, and each requires different paperwork and enrollment steps.
How do Medicaid waivers enable family caregiver payments?
Medicaid waivers—often referred to as HCBS waivers—allow states to deliver long-term services and supports in community settings rather than institutions, and many waivers include a self-direction option that permits the care recipient to hire and manage their own caregiver. Self-direction typically establishes the care recipient or a designated employer-authority who hires caregivers, sets schedules, and authorizes payment; some states permit hiring qualified family members within that framework. The waiver process requires a needs assessment, a care plan that specifies services, and administrative enrollment steps that can include background checks and caregiver training. This structure makes waivers a key mechanism for enabling family members to be compensated when state rules allow it.
What other programs fund caregiver payments, including VA benefits and paid family leave?
Beyond Medicaid waivers, other programs provide payment or wage-replacement options to caregivers depending on circumstance and eligibility. The VA offers certain caregiver supports and benefit streams for eligible veterans that can include paid services or contracted home care, while state paid family leave programs provide temporary wage replacement for workers who take leave to care for a family member but do not necessarily create a caregiver-employer relationship. Additional supports such as tax credits, local Area Agency on Aging resources, and nonprofit grants can also offset caregiving costs. Knowing which program aligns with a caregiver’s employment status, veteran status, or care recipient needs helps identify the most practical funding route.
How to Apply for Respite Grants and Caregiver Vouchers: Step-by-Step Process
Applying successfully requires a structured approach: identify the right program, assemble required documents, complete intake and assessments, and follow up persistently to resolve requests for additional information. A clear timeline and checklist reduce delays and increase the likelihood of approval. Below is a compact how-to roadmap with typical timelines and advice for avoiding common obstacles so caregivers can move from application to payment as efficiently as possible.
Identify the correct program and responsible agency based on the care recipient’s status and residency.
Gather essential documentation including medical records, proof of residence, income verification (if required), and a current care plan.
Submit intake forms to the issuing agency and schedule required assessments (e.g., level-of-care evaluations or veteran eligibility reviews).
Respond promptly to requests for additional information and enroll in training if the program requires caregiver qualifications.
Complete enrollment and set up payment or voucher redemption procedures; track hours and services as required.
These steps outline a common pathway, but timelines vary: intake to assessment often takes 2–8 weeks, approvals for waivers can take months, and voucher disbursement schedules differ by agency. Persistence, organized records, and strong documentation are the most effective techniques to accelerate approvals.
Educate family caregivers on eligibility and process for getting paid, and guide them to apply for Paid.care's services.
Paid.care assists family caregivers through eligibility checks and application guidance; caregivers who want targeted help with enrollment can use Paid.care’s check-eligibility flow to confirm potential program matches. Paid.care’s role is to clarify which state programs a caregiver might qualify for and to point to next administrative steps while keeping the application roadmap focused on official agency requirements. This bridge helps caregivers prioritize documentation and choose the most promising application pathway.
What documents and steps are required to apply for caregiver payment programs?
Most applications require a consistent core of documentation and administrative actions, and preparing this packet in advance reduces processing time and follow-up requests. Essential documents commonly include medical records or a physician statement verifying the care recipient’s condition, proof of residency (utility bill or state ID), identification for the caregiver and care recipient, and any income or asset statements if the program is means-tested. The application sequence typically follows intake → assessment/care plan → approval → enrollment → payment setup, and caregivers can shorten delays by providing complete medical notes and clear care schedules at intake. Keeping a master folder—physical or digital—with all required documents helps ensure quick responses to agency queries and supports smoother enrollment.
How does Paid.care simplify the application and payment process for family caregivers?
Paid.care provides support services that map directly to common bottlenecks in caregiver payment programs: eligibility screening, training, ongoing care coaching, and payment administration. Paid.care performs eligibility checks for Medicaid/HCBS/consumer-directed/veteran-directed/respite/paid family leave programs to identify which pathways may apply to a given caregiver and care recipient. In addition, Paid.care offers caregiver training and free dedicated care coaching with 24/7 support to help caregivers meet program requirements and maintain care quality. The company also supports payment logistics by enabling weekly payments and providing a mobile app for management and hour tracking, which helps caregivers document services and receive timely compensation. Together, these features aim to simplify enrollment and reduce administrative friction for families pursuing paid caregiving arrangements.
Where to Find State-Specific Respite Grant and Medicaid Waiver Programs
State programs are the operational front line: eligibility details, rate-setting, and allowable caregiver relationships are set locally, so locating state-specific program names and contact points is essential for a successful application. For caregivers in Indiana, Michigan, and Illinois, knowing the relevant waiver names and where to begin intake (state Medicaid agency, Area Agency on Aging, or veteran services office) speeds enrollment. This section gives a compact state-by-state reference to highlight program names and practical first steps.
What respite and caregiver payment programs are available in Indiana, Michigan, and Illinois?
In Indiana, Michigan, and Illinois, Medicaid HCBS waivers are the primary route for sustained caregiver payments when states permit self-direction, while state and local respite grants or vouchers supply short-term relief for families needing temporary support. Each state uses clinical assessments and enrollment processes to determine level-of-care and service authorization, and local Area Agencies on Aging often administer or coordinate respite funding at the county level. Caregivers should begin with the state Medicaid intake line or their local AAA to request an assessment and learn whether the program allows hiring family members or provides vouchers. Preparing medical documentation and a clear care plan before intake reduces processing time and clarifies the best program match.
How will upcoming expansions to Tennessee, Ohio, and South Dakota affect caregiver payment options?
Planned expansion of services and supporting organizations to additional states increases geographic availability of some enrollment assistance and consumer-directed options, which may improve access to eligibility checks and application support in those regions. Caregivers in Tennessee, Ohio, and South Dakota should watch for state-specific rollouts, official guidance on waiver enrollment, and local Area Agency on Aging communications that announce when new supports become available. In the interim, caregivers can prepare by gathering medical documentation and drafting a care plan to be ready to apply when eligibility screening and application assistance are offered in their state.
At the end of this section, caregivers who want help confirming program matches can Check Eligibility with Paid.care; Paid.care currently assists families in Indiana, Michigan, and Illinois and is expanding support to Tennessee, Ohio, and South Dakota. This short navigational recommendation helps caregivers find the right starting point without replacing official agency intake.
What Are Common Questions About Respite Grants and Caregiver Vouchers?
Caregivers often ask whether family members can be paid, how much they can expect to receive, and which programs make payment most likely; concise, direct answers help families prioritize applications and set realistic expectations. This FAQ-style section addresses the most common PAA-style queries and provides practical pointers about verification resources and pay variability.
Can a family member get paid for caregiving through government programs?
Yes—under specific programs and conditions, family members can be paid for caregiving, most commonly through Medicaid HCBS waivers that include self-direction or certain state voucher programs that permit family hires. Eligibility hinges on program rules: some allow family members as paid caregivers after meeting training, background check, or documentation requirements, while others restrict payments to non-relative providers. Caregivers should verify allowable relationships with the state Medicaid agency, the Area Agency on Aging, or the administering agency for the voucher or grant to confirm whether hiring a family member is permitted in their program. Preparing required paperwork and completing any mandated training helps satisfy program conditions for paid family caregiving.
How much do family caregivers typically get paid under these programs?
Payment varies widely by state, program type, and care level—some programs set hourly rates, others provide daily stipends or voucher values, and Medicaid waiver rates are state-determined and often tied to assessed needs. For example, program pay can range from modest hourly supports to significantly higher compensation in some states; Paid.care’s example compensation in Indiana exceeds $250 per day in certain circumstances, illustrating the potential variance across programs and jurisdictions. Factors that drive pay include the care recipient’s assessed level-of-care, state rate-setting, allowable caregiver relationships, and program budget limits. To estimate realistic compensation, caregivers should consult program rate schedules or use pay calculators where available and track hours carefully for accurate reimbursement under voucher or waiver arrangements.
Paid.care encourages caregivers to use eligibility checks to confirm which funding pathways are available and to prepare documentation that matches program requirements. This final reminder aims to help families take a concrete next step toward applying with the proper paperwork and program choice in hand.
Prepare core documents: medical notes, proof of residency, IDs, care plan.
Contact the right agency: state Medicaid intake, Area Agency on Aging, or veteran services.
Track services: keep a log of hours and tasks for approvals and payment reconciliation.
This combined checklist completes the article’s actionable guidance and creates a bridge from knowledge to application without replacing the official agency process.
Identify the program that fits your situation and residency.
Assemble required medical and identity documents upfront.
Respond quickly to agency requests and enroll in required training or assessments.
This combined checklist completes the article’s actionable guidance and creates a bridge from knowledge to application without replacing the official agency process.
FAQs
-
Respite grants and vouchers are financial assistance programs that help family caregivers pay for short-term, temporary breaks from caregiving. Instead of you paying fully out of pocket, a grant or voucher can cover all or part of the cost of in-home respite, adult day programs, overnight stays in a facility, or camp/short-term programs for children with disabilities. The goal is to prevent caregiver burnout and keep your loved one safely cared for while you rest, work, or handle other responsibilities.
-
Depending on your situation, you may find respite help through:
Your local Area Agency on Aging (AAA) or Aging & Disability Resource Center (ADRC)
State Lifespan Respite programs or state caregiver support programs
Medicaid waivers that include respite as a covered service
Developmental disability or mental health agencies (for children or adults with disabilities)
Disease-specific organizations, like Alzheimer’s, Parkinson’s, cancer, or ALS associations
Tribal health or elder services programs, for Native American/Alaska Native families
Nonprofits such as Easterseals, local faith-based charities, or community foundations
Most families will start by calling their AAA/ADRC or state respite program and asking, “Do you offer respite grants or vouchers for family caregivers, and how do I apply?”
-
Eligibility rules vary widely, but programs commonly look at:
The care recipient’s age (for example, older adults 60+ or children with special health needs)
A documented disability, chronic illness, or cognitive impairment
The level of care needed (help with bathing, dressing, constant supervision, etc.)
Income or financial need, in some cases
Whether a family caregiver is providing unpaid care at home
Some programs are very targeted (e.g., caregivers of people with dementia), while others are open to any unpaid caregiver who meets basic guidelines. Many have limited funding, so waitlists are common—applying early is key.
-
Respite grants and vouchers typically cover short-term relief, not full-time care. Depending on the program, funds might pay for:
In-home respite aides who come to your home for a few hours or days
Adult day health or social day programs so your loved one is supervised during the day
Short stays in a nursing facility, assisted living, camp, or group home for planned respite weekends or emergencies
Specialized respite programs (for children with autism, complex medical needs, or behavioral challenges)
Some programs pay providers directly; others give you a voucher or reimbursement after you submit receipts for approved respite services.
-
To make the process smoother:
Gather documentation: diagnoses, care needs, proof of income (if required), and any existing care plans.
Be specific when describing how much help you provide and how caregiving affects your health, work, or finances.
Ask whether the program uses approved providers or allows you to hire your own respite worker.
Keep records of all respite hours and receipts if you’re reimbursed rather than prepaid.
Reapply or follow up before your authorization period ends, so you don’t lose access unexpectedly.
If you’re overwhelmed, ask for help from a care coordinator, social worker, or local caregiver support program—they can often point you to multiple respite funding sources and help with the paperwork.