Paid Family Care Rules for Overnight and On-Call Hours: Eligibility, Compensation, and Application Guidance
Family caregivers who provide overnight supervision or remain on-call face unique eligibility and pay rules that differ across programs and states. This guide defines "overnight" and "on-call" care, explains how Medicaid waivers, paid family leave, and veteran-directed programs may authorize payment for extended hours, and maps the rules that affect compensation and legal classification. Many caregivers wonder whether sleep time counts as paid work, how overtime is triggered, and what documentation is required to get paid; this article addresses those questions with practical steps. You will learn the core eligibility criteria, the mechanics of compensation calculation including sleep-time rules under the FLSA, a step-by-step application process, and state-specific notes for Indiana, Michigan, and Illinois. Practical lists, comparison tables, and examples will help you collect the right records and present them to program managers. Finally, the article outlines how Paid.care can support eligibility checks, care coaching, time tracking, and weekly payments for those pursuing paid family care.
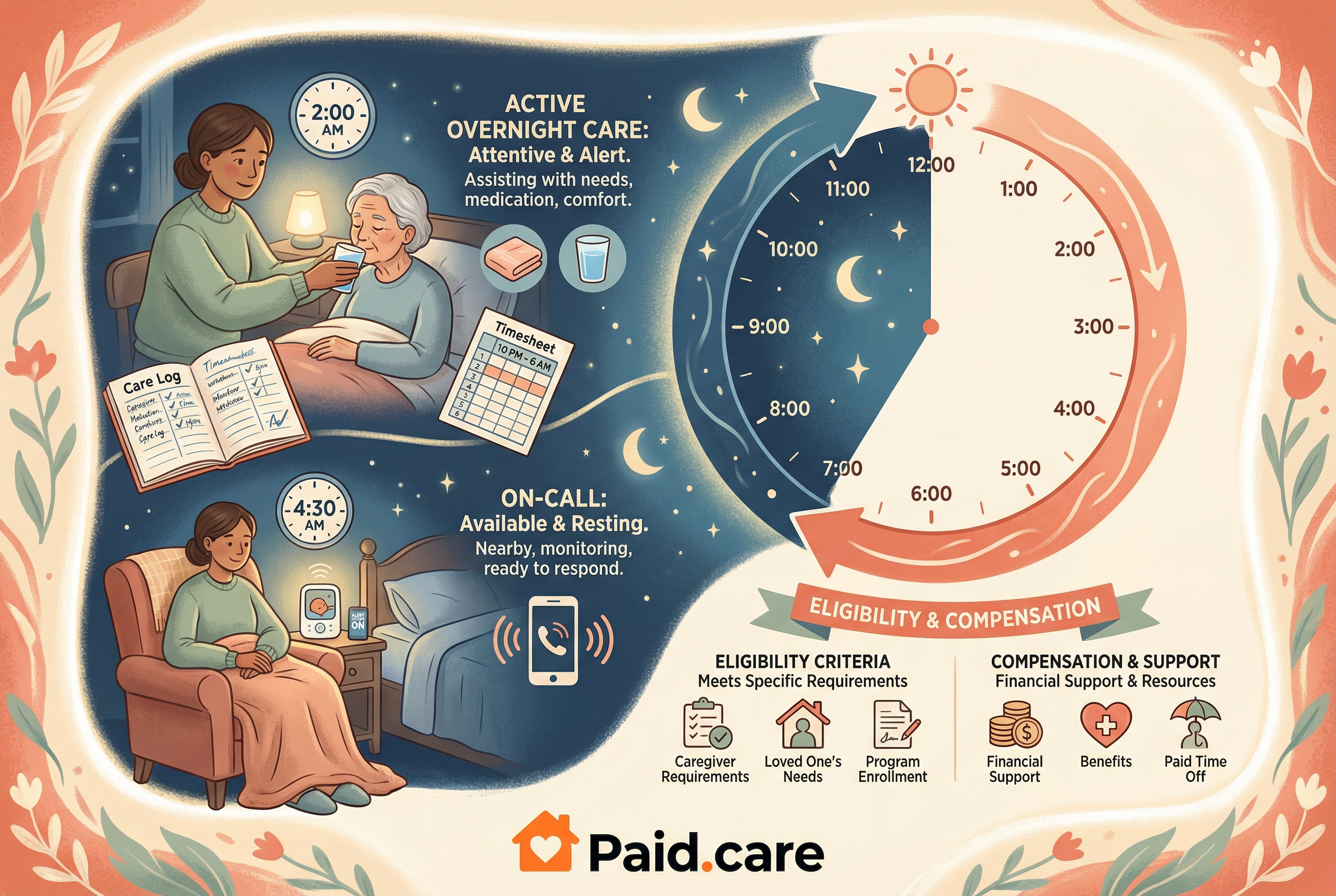
What Are the Eligibility Requirements for Paid Overnight and On-Call Family Care?
Eligibility for paid overnight or on-call family care depends on program type, the care recipient’s assessed needs, and caregiver relationship or residency requirements. In general, programs that pay family caregivers require a certified need for assistance during nights or unpredictable hours, a designated caregiver relationship (family or legal guardian), and an approved care plan that authorizes paid hours. These criteria ensure that payment aligns with documented service needs and program rules, and they reduce the risk of misclassification for both the caregiver and the payer. Understanding these baseline elements prepares applicants to gather medical assessments, relationship verification, and plan approvals before submitting an application, which speeds the review process and clarifies expected compensation. The next subsections examine how Medicaid waivers and state paid family leave handle overnight or on-call hours in practical terms.
For caregivers who want quick confirmation of whether they may qualify, Paid.care offers eligibility-check assistance and free care coaching to review basic criteria and next steps. Paid.care’s team helps summarize program options and guide caregivers toward the right program pathway when overnight or on-call needs are present.
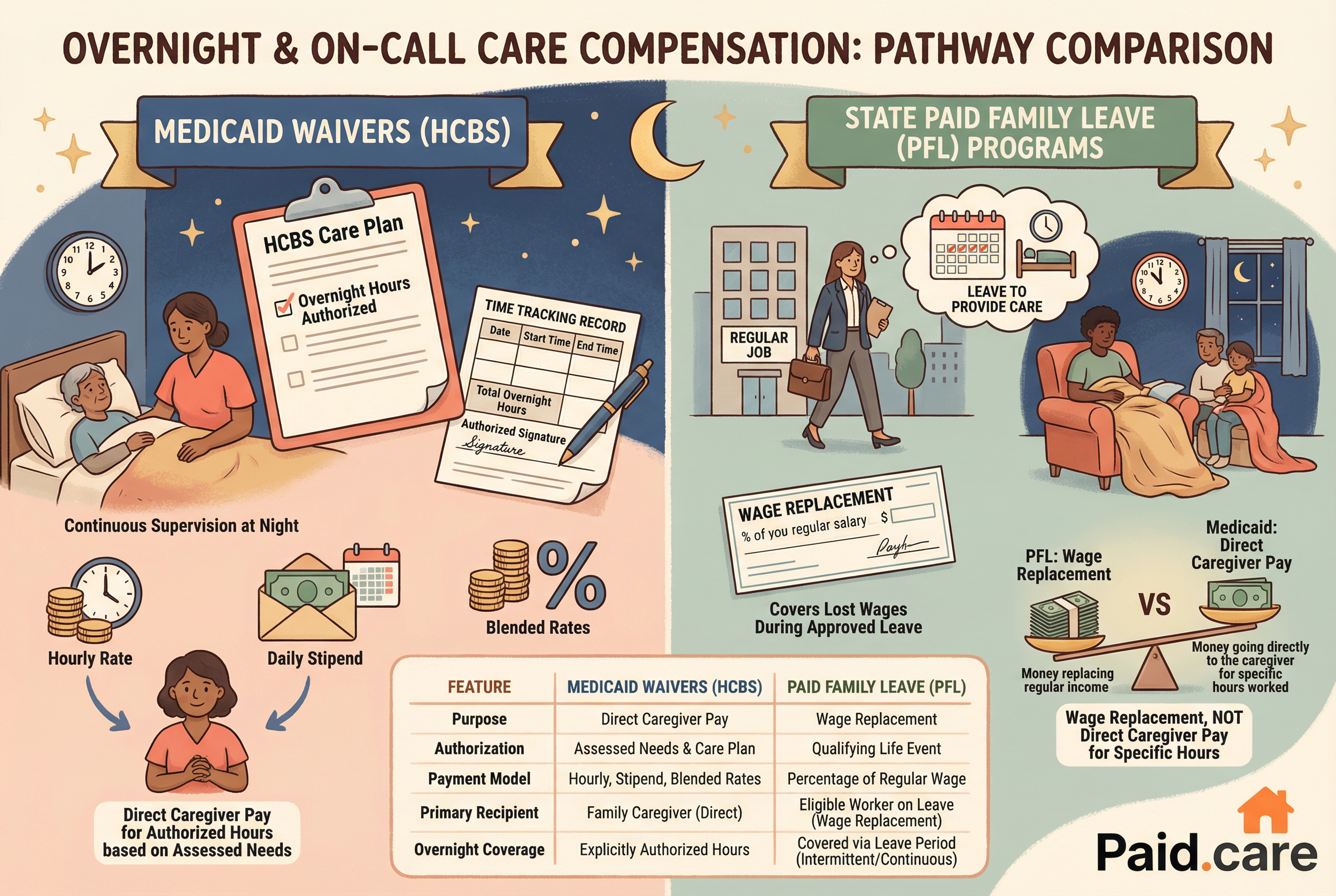
How Do Medicaid Waivers Cover Overnight and On-Call Care?
Medicaid waivers, such as HCBS waivers and self-directed programs, can fund family caregivers for overnight and on-call shifts when the care plan explicitly authorizes those hours based on assessed needs. Waiver programs operate by assessing the care recipient’s functional needs, creating a person-centered care plan, and approving services and hours that can include continuous supervision, intermittent overnight checks, or on-call coverage. In consumer-directed or self-directed models, the care recipient or their representative can hire family members as paid caregivers where state rules permit, which often requires caregiver enrollment and background checks. Documentation typically includes clinical assessments, a written care plan specifying overnight responsibilities, and time-tracking records to verify billed hours. These procedural steps lead directly to questions about how pay is calculated and how sleep time is treated under federal labor standards.
Different waivers use different payment models—hourly, daily stipends, or blended rates—so verifying the waiver’s payment approach is essential before accepting overnight assignments.
Which State Paid Family Leave Programs Include Overnight Care?
State paid family leave (PFL) programs generally provide wage replacement to eligible workers who take leave to care for a family member, but they do not typically pay a caregiver directly to work overnight shifts for another person. PFL covers the caregiver’s lost wages during leave for qualifying events and sometimes allows intermittent use that could include overnight care performed by the family member who is on leave. Because PFL is wage replacement rather than a direct employer-pay model, it differs from Medicaid waivers or veteran-directed programs that can authorize payment to a designated caregiver under a care plan. Eligibility and allowable uses vary by state, so it is important to check program-specific definitions of caregiving and acceptable leave uses when planning overnight or on-call coverage. Understanding this distinction helps families decide whether to pursue a wage-replacement leave or an authorization to pay a family member as a caregiver.
Knowing whether you need direct caregiver pay versus wage-replacement influences the application pathway you will follow next, and that leads into how compensation is calculated across programs.
How Is Compensation Calculated for Overnight and On-Call Family Caregivers?
Compensation for overnight and on-call family care can take several forms—hourly wages, daily stipends, or blended rates that separate active care from sleep or standby hours—and the final pay depends on program rules and labor law interpretations. Factors that determine compensation include whether sleep time is considered compensable under the Fair Labor Standards Act, whether the caregiver is classified as a bona fide live-in employee, and state-specific mandates for overtime or minimum standby pay. Programs may set different rates for active night interventions versus passive supervision, and they often require precise time-tracking to support billable hours. A clear calculation approach typically combines hours of active care, allowable sleep or standby credit, and overtime pay when weekly thresholds are exceeded, so caregivers should maintain detailed records to ensure correct payment.
What Are the Fair Labor Standards Act Rules for Caregiver Overtime and Sleep Time?
Under the Fair Labor Standards Act (FLSA), employers must pay minimum wage and overtime for non-exempt employees, and the Department of Labor’s guidance clarifies when sleep time and on-premises standby time is compensable. Sleep time is generally non-compensable if the employee is free to sleep and provided adequate sleeping facilities, but time is compensable if the employee is required to perform duties or if interruptions prevent uninterrupted sleep. The bona fide live-in caregiver exemption may apply in certain circumstances but is narrowly defined and varies in application; misclassification risks unpaid overtime claims if the exemption is applied incorrectly. Good recordkeeping—documented sleep periods, interruptions, and active care episodes—supports proper classification and defends pay calculations during audits. Understanding these federal baselines helps caregivers and program administrators structure pay and schedules that comply with labor law while ensuring appropriate compensation.
Clear documentation of when a caregiver was actively engaged versus on-call but resting directly affects whether those hours are included in overtime calculations.
How Do Indiana, Michigan, and Illinois Differ in On-Call and Overnight Pay?
Indiana, Michigan, and Illinois each have nuances in how they apply program rules and labor standards to overnight and on-call family caregiving, especially within Medicaid waiver and state labor contexts. In many cases, state Medicaid waivers determine whether family members may be hired as paid caregivers and set pay rates or caps, while state labor departments interpret overtime and sleep-time rules in line with federal guidance but may add clarifying regulations. For example, structured family caregiving options and self-directed programs are available in these states with differing enrollment processes and approved pay models; some states authorize daily stipend models while others prefer hourly rates for extended care. Caregivers should consult state Medicaid waiver documents and labor offices for definitive guidance and keep program contacts handy for eligibility and pay questions. These state-specific differences mean the next section’s application steps must be tailored to the program and state the caregiver pursues.
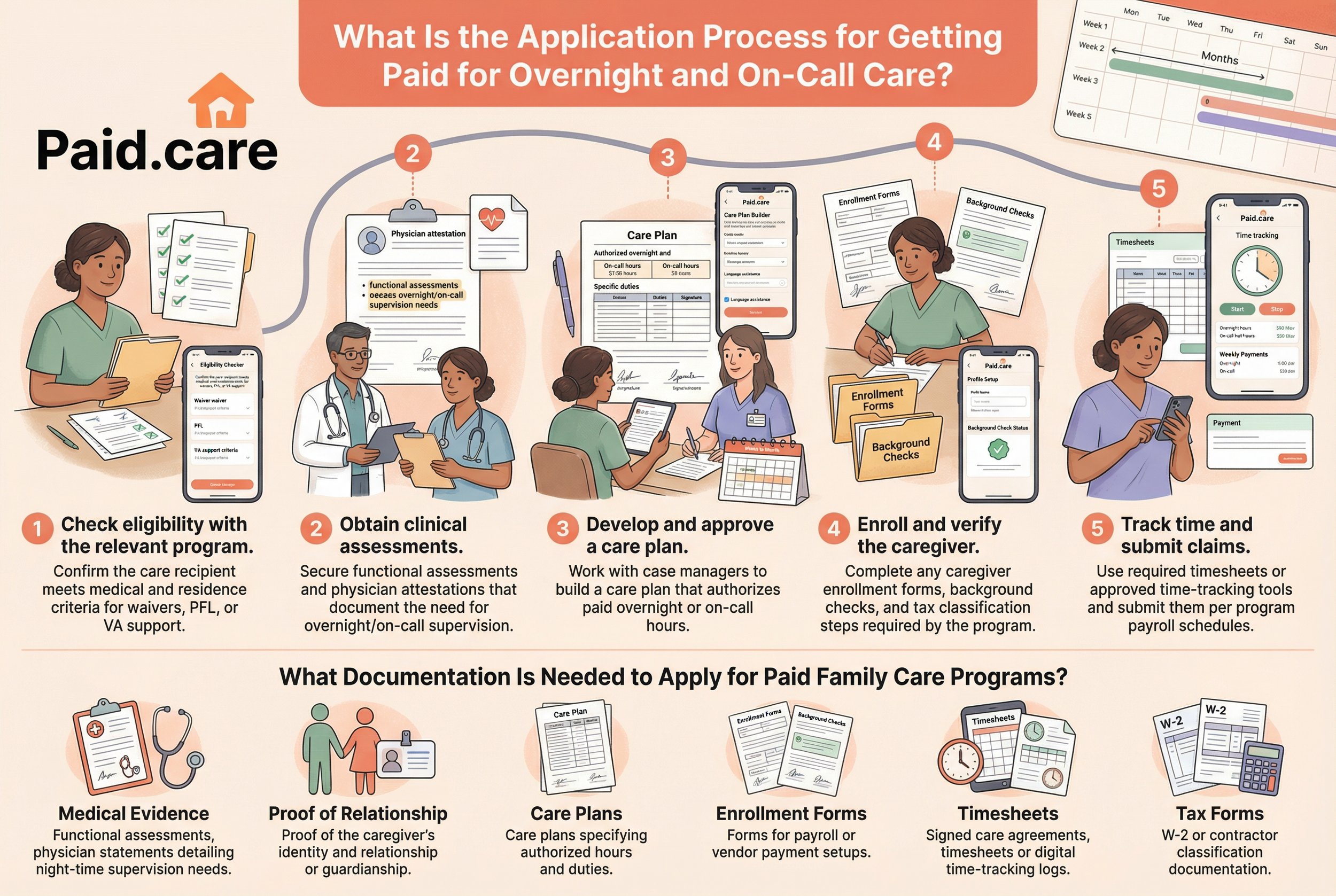
What Is the Application Process for Getting Paid for Overnight and On-Call Care?
The application process for paid overnight and on-call care generally follows a clear workflow: confirm program eligibility, obtain clinical assessments, develop an authorized care plan, enroll the caregiver, and submit time records for payment. Each step requires specific documentation and program-level approvals, and timelines can vary from weeks to months depending on assessment and administrative queue lengths. Preparing complete medical evidence, a clear care agreement that defines overnight responsibilities, and consistent time-tracking records reduces back-and-forth with program managers and speeds payment authorization. The numbered list below summarizes the core application steps to target featured-snippet style guidance and provide a quick checklist for caregivers starting the process.
Check eligibility with the relevant program: Confirm the care recipient meets medical and residence criteria for waivers, PFL, or VA support.
Obtain clinical assessments: Secure functional assessments and physician attestations that document the need for overnight/on-call supervision.
Develop and approve a care plan: Work with case managers to build a care plan that authorizes paid overnight or on-call hours.
Enroll and verify the caregiver: Complete any caregiver enrollment forms, background checks, and tax classification steps required by the program.
Track time and submit claims: Use required timesheets or approved time-tracking tools and submit them per program payroll schedules.
Applying these steps in order reduces delays and clarifies when pay will begin; the next subsection lists the documentation typically needed to complete these steps.
Paid.care supports caregivers across this workflow by offering documentation review, profile setup assistance, and guidance on building an eligible care plan, and the Paid.care App supports time tracking and weekly payments for enrolled caregivers.
What Documentation Is Needed to Apply for Paid Family Care Programs?
Successful applications for paid family care programs commonly require a combination of medical evidence, proof of relationship or guardianship, and administrative documentation that sets up payment and reporting. Typical items include functional assessments or physician statements detailing night-time supervision needs, care plans that specify authorized hours and duties, proof of the caregiver’s identity and relationship, and enrollment forms for payroll or vendor payment setups. Programs may also require signed care agreements, timesheets or digital time-tracking logs, and tax or payroll documentation for W-2 or contractor classification depending on the program’s employment model. Maintaining organized copies of these documents and ensuring timely submission reduces requests for additional information and helps secure approvals faster. The subsequent subsection explains how technology can help collect and present these records consistently.
How Does the Paid.care App Support Time Tracking and Payment for Extended Hours?
The Paid.care App provides practical tools that map directly to the documentation and time-tracking requirements programs often demand for overnight and on-call pay authorization. Caregivers can use the app’s eligibility checker to confirm potential program matches, chat with care coaches who advise on documentation and care plan language, and build a plan that identifies billable overnight duties. Time-tracking features capture active care interventions and sleep/standby periods in a structured format that supports payroll validation, and Paid.care processes weekly payments to enrolled caregivers based on validated entries. Using a single tool for eligibility checks, care plan building, and time recording reduces fragmentation and creates an auditable trail of care delivery that aligns with program reporting needs. This integrated workflow directly supports faster pay cycles and reduces disputes over compensable hours.
These operational supports demonstrate how technology and coaching combine to simplify the application-to-pay cycle and lead into real-world caregiving scenarios where overnight care matters most.
What Are Common Caregiving Scenarios Involving Overnight and On-Call Hours?
Overnight and on-call caregiving appears in several common scenarios—24/7 care for children with complex medical needs, dementia night supervision for older adults, and intermittent overnight support following acute hospital discharges. Each scenario creates different expectations for active interventions versus passive supervision, and program rules typically tie payment to documented clinical need and frequency of interventions. For children with high needs, waivers often allow continuous paid care when the care plan and functional assessment support round-the-clock supervision; dementia care may be compensated differently if frequent nighttime interventions are required. Understanding scenario-specific documentation expectations helps families select the right program pathway and ensures that time-tracking accurately reflects billable activity. The following examples illustrate how rules apply in practice and prepare caregivers for program discussions.
The next subsections break down how 24/7 child care and dementia night shifts are typically compensated under common program models.
How Is 24/7 Care for Disabled Children Compensated?
When a child has complex medical or behavioral needs that require continuous supervision, Medicaid waivers and self-directed programs often authorize paid family caregiving for extended hours including overnight coverage. Compensation models for 24/7 care can include hourly rates for active care, flat daily stipends for continuous supervision, or blended approaches that recognize periods of sleep versus active intervention. Care plans and functional assessments must document the level of need, and programs frequently require detailed time records to support claims for long shifts or overnight coverage. Families should coordinate with case managers to ensure the approved plan reflects typical nightly interventions and to confirm whether respite or supplemental supports are available to reduce caregiver burden. Proper authorization and accurate time documentation are essential to convert intensive caregiving responsibilities into sustainable paid arrangements.
Documented evidence of nighttime interventions and a clearly authorized care plan make reimbursement for 24/7 care more defensible in audits and appeals.
What Are the Guidelines for Dementia Caregiver Compensation During Night Shifts?
Dementia caregiving at night often involves a mix of passive supervision and unpredictable active episodes such as wandering, sundowning agitation, or toileting assistance, and pay depends on the frequency and intensity of those interventions. Programs typically compensate active interventions when they occur and may treat prolonged passive supervision differently depending on whether the caregiver is required to remain awake or available on the premises. Documentation that logs each episode, the caregiver’s response, and clinical notes that justify ongoing night supervision strengthens claims for higher paid hours. Caregivers should work with clinicians to include night-risk behaviors in the care plan and to get concrete language that explains why night monitoring is medically necessary. Accurate recordkeeping of episodic interventions and clinical corroboration supports appropriate compensation for nighttime dementia care.
These scenario-specific approaches underscore the need to navigate labor rules and state regulations carefully, which is the focus of the next major section.
How Can Family Caregivers Navigate Labor Laws and State Regulations for Overnight Pay?
Navigating labor laws and state regulations for overnight pay requires understanding federal baselines under the FLSA, how sleep-time deductions operate, and where state-specific rules impose additional obligations or offer alternative pay models. Families should evaluate whether caregivers are employees or independent providers under program rules, document on-premises requirements that make sleep time compensable, and consult state Medicaid and labor resources for nuances that affect overtime, minimum wage, and live-in exemptions. Recordkeeping practices—clear timesheets, sleep logs, and incident notes—are essential for compliance and for defending pay calculations during audits.
What Are the Sleep Time Deduction Rules for Live-In Family Caregivers?
Sleep time deductions allow employers to exclude periods of uninterrupted sleep from compensable hours under narrow conditions, but the rules require that employees be completely relieved of duties and provided adequate sleeping facilities. If a caregiver is required to remain on-call or to respond to interruptions, those sleep periods become compensable and must be included in paid hours. For live-in family caregivers, distinguishing between bona fide live-in status and other on-premises arrangements is critical because misclassification can trigger back-pay and overtime liabilities. Practical recordkeeping—explicitly noting sleep start and end times, interruptions, and active responses—supports lawful deductions and demonstrates compliance. Caregivers and program administrators should document expectations in the care agreement to reduce ambiguity when sleep deductions are applied.
Careful recording of interruptions and active duties during the night directly affects whether sleep time can be legitimately excluded from pay calculations.
Which States Require Compensation for On-Call Hours and How Is It Calculated?
States vary in when on-call time is compensable: time spent on the employer’s premises or time with limited freedom of movement often counts as paid time, while remote standby with no restrictions may not. Calculation methods include hourly rates for each hour on-call, partial pay for standby time, or inclusion of on-call hours in overtime calculations when weekly thresholds are exceeded. Documentation that demonstrates the location, response expectations, and frequency of required responses helps determine compensability and the appropriate calculation method. When on-call duties demand immediate responses or restrict the caregiver’s freedom, treating the hours as compensable reduces legal risk and better reflects actual work performed. The next section examines how practical services can streamline these compliance steps for caregivers seeking paid overnight or on-call compensation.
Clear agreements that define required response times and location expectations help programs and caregivers agree on whether on-call periods are payable.
How Does Paid.care Assist Family Caregivers with Overnight and On-Call Compensation?
Paid.care is a lead generation and information hub that helps family caregivers navigate payment pathways for overnight and on-call care through eligibility checks, free care coaching, and technology that supports time tracking and weekly payments. The service assists families in identifying potential programs—Medicaid waivers, HCBS/self-directed programs, veteran-directed care, and paid family leave—then guides caregivers through documentation requirements and care plan language that supports night or on-call authorization. Paid.care highlights competitive pay models in service areas and, where applicable, W2 employment pathways that can include higher daily rates (for example, program examples show competitive rates in Indiana) and sign-on incentives for qualified caregivers. By combining coaching, app-driven recordkeeping, and a weekly payment cadence, Paid.care aims to reduce administrative friction and help caregivers convert approved hours into timely compensation.
This business-focused overview shows how integrated coaching and technology support the steps described earlier and sets up the more detailed services offered below.
What Support and Coaching Does Paid.care Provide for Eligibility and Application?
Paid.care provides free care coaching that walks caregivers through eligibility screening, documentation preparation, and the application submission process to reduce errors and speed approvals. Coaches help interpret waiver language, advise on the clinical evidence needed to justify overnight or on-call hours, and assist in building care plans that align with program rules and caregiver availability. The service includes training resources and enrollment support for caregivers who need to complete required background checks or payroll setup, and coaches are available to answer procedural questions that commonly delay approvals. This hands-on assistance is designed to increase approval rates and shorten the time between application submission and first payment.
Coaching paired with clear documentation practices addresses common application pitfalls and reduces the administrative burden on families.
How Does Paid.care Ensure Timely Weekly Payments for Extended Care Hours?
Paid.care’s operational workflow validates time entries from the Paid.care App, resolves disputes through a documented dispute resolution process, and processes weekly payroll for enrolled caregivers based on validated hours. Time-tracking entries that distinguish active care from sleep or standby periods are reviewed and matched against the approved care plan before payments are released, and caregivers receive weekly payouts that reflect validated entries. Paid.care also stores documentation for audit support and provides 24/7 assistance to troubleshoot eligibility or pay questions that could delay payment. These steps create an auditable trail and predictable payment cadence, which helps caregivers rely on steady income when providing overnight or on-call services.
A predictable validation-to-pay workflow reduces payment uncertainty and helps caregivers focus on care delivery rather than administrative follow-up.
Would you like to find out exactly which Ohio program you qualify for and see your estimated pay rate? Visit Paid.Care today to start your free eligibility assessment.
FAQs
-
The Rule: Generally, under federal labor standards (FLSA), if you are on duty for 24 hours or more, up to 8 hours of "sleep time" may be deducted from your pay—but only if you are provided adequate sleeping facilities and can enjoy at least 5 hours of uninterrupted sleep. If you are interrupted to provide care and get less than 5 hours of sleep, the entire period typically must be treated as paid work time.
Application Guidance: Keep a meticulous log of every time you wake up to assist the care recipient. If interruptions are frequent, provide this log to your case manager to prove that a "sleep deduction" should not apply.
-
The Eligibility Criteria: Insurance and Medicaid programs rarely pay for overnight care strictly for "safety monitoring" (just being there "in case"). To be eligible, there must be a documented medical necessity, such as the need for repositioning every two hours to prevent bedsores, assistance with toileting/incontinence, or managing wandering behaviors due to dementia.
Application Guidance: Ask the recipient’s doctor to explicitly write a prescription or letter of necessity stating specific overnight tasks (e.g., "Patient requires tracheal suctioning at 2 AM and 4 AM"). Vague requests for "supervision" are often denied.
-
The Rule: The distinction often comes down to "Engaged to Wait" vs. "Waiting to be Engaged." If you are required to stay on the premises and your freedom is significantly restricted, you are likely "Engaged to Wait" and should be paid for those hours. If you are allowed to leave, run errands, and use the time effectively for yourself while waiting for a call, you might not be eligible for hourly pay until you actually respond to a call.
Application Guidance: Review your caregiver contract or state Medicaid waiver handbook. If you are not allowed to leave the house during on-call hours, ensure you are billing this as active duty time.
-
The Compensation Structure: This varies by program. Some agencies pay the standard hourly rate for all waking hours. Others may offer a "flat rate" or "per diem" for overnight shifts, particularly for live-in caregivers. However, this flat rate must still average out to at least the applicable minimum wage for all hours worked when divided.
Application Guidance: Before accepting an overnight schedule, calculate the total pay divided by the hours you are required to be there. If it falls below minimum wage, the pay structure may be in violation of labor laws.
-
The Rule: Yes. In many states and under federal law, live-in domestic service workers may be exempt from overtime pay requirements (meaning they get straight time for hours over 40), or the rules for calculating hours worked may differ significantly from non-resident caregivers.
Application Guidance: Be cautious before officially changing your status to "live-in" (residing there permanently or for extended periods). While it offers housing benefits, you may lose overtime premiums. Clarify with your payroll department exactly how "live-in" status affects your time-and-a-half eligibility.