Paid Family Care Pay Gaps During Program Transitions: How to Ensure Continuous Caregiver Payment
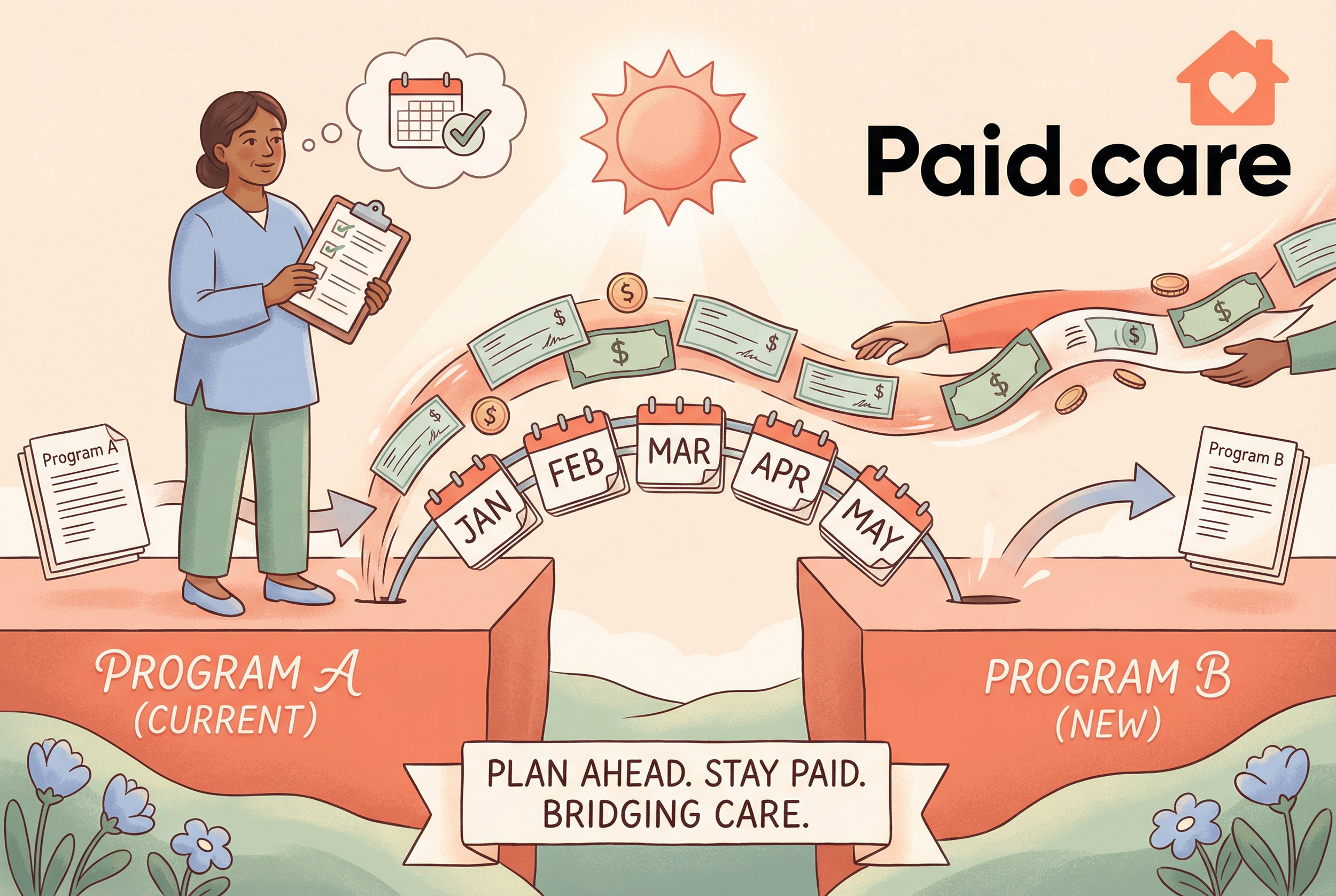
Many family caregivers experience "pay gaps"—periods when compensation for in-home care is delayed, reduced, or halted—during program transitions, and understanding these interruptions is the first step to preventing income shocks. This guide explains what pay gaps are, why they happen during transitions such as Medicaid redetermination or waiver changes, and what practical steps caregivers can take to keep payments flowing. Readers will learn the administrative and policy mechanisms that interrupt pay, concrete pre- and post-transition actions to minimize risk, and where alternative programs and tools fit into a continuity plan. The article also maps eligibility changes, compares supplemental programs, and highlights specific operational tactics such as documentation checklists, appeals steps, and communication strategies with agencies. Finally, we cover how specialized services can operationalize prevention strategies so caregivers can stabilize cash flow while navigating program complexity.
Why Do Pay Gaps Occur During Medicaid Caregiver Payment Transitions?
A pay gap during a Medicaid-related transition happens when program administration, eligibility re-evaluations, or policy adjustments interrupt the normal flow of compensation to family caregivers, creating sudden income shortfalls. These interruptions occur because payments rely on timely eligibility verification, consistent billing and vendor processing, and state-level policy continuity; any break in those links triggers pause or delay.
Understanding the common causes helps caregivers prioritize which administrative levers to control and which risks to escalate quickly to agencies. The next section lists typical causes and follows with a compact table mapping cause to immediate caregiver impact and typical mitigation.
Common causes of pay gaps include the following administrative and policy drivers:
Administrative delays in processing applications or invoices that leave caregivers unpaid during backlog periods.
Medicaid redetermination outcomes that suspend payments until eligibility is re-established or appealed.
State policy changes or rate restructures that alter pass-through rules or vendor payment timelines.
Documentation gaps or mismatches between caregiver/provider records and beneficiary files that trigger hold periods.
These causes often overlap, so caregivers should prepare for combinations of delay, suspension, or reduced rates and then prioritize actions that address the most likely root cause.
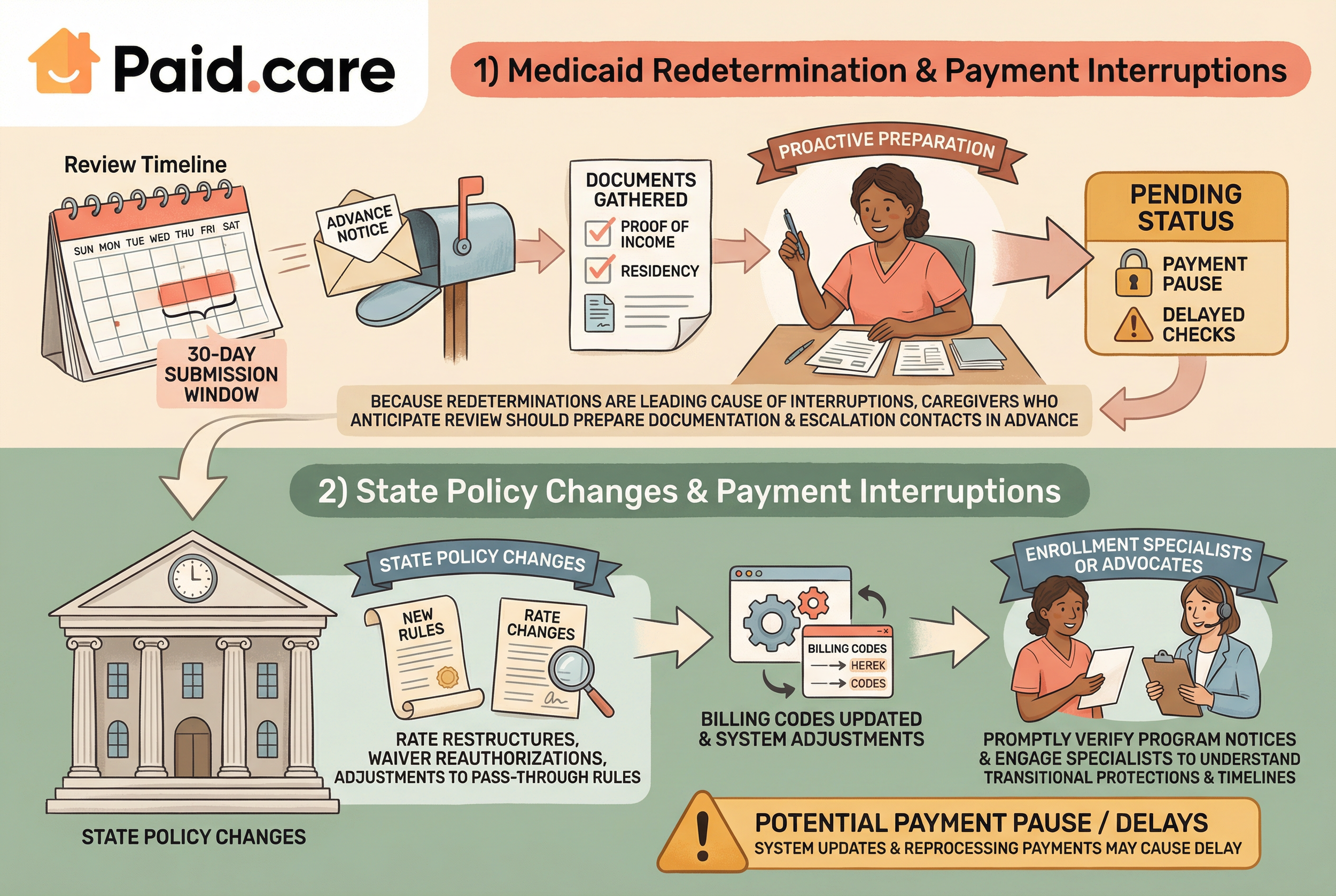
What Is Medicaid Redetermination and How Does It Affect Caregiver Payments?
Medicaid redetermination is the periodic review process state Medicaid agencies use to confirm a beneficiary still meets eligibility requirements, and it affects caregiver payments because a beneficiary’s suspended or terminated coverage directly pauses any associated paid family care benefits. The process typically involves advance notices, document submission windows, and a defined review period; missed deadlines or incomplete submissions can instantly move a beneficiary into "pending" status, which often stops payments to the caregiver. For example, when eligibility verification requires proof of income or residency and those documents are delayed in transit, a caregiver may see a one-to-two pay cycle suspension while the agency resolves the file.
Understanding typical timelines—advance notice, 30-day submission windows, and potential appeals—helps caregivers forecast when to submit documents and when to escalate if payments are delayed.
Because redeterminations are a leading cause of interruptions, caregivers who anticipate an upcoming review should prepare documentation and escalation contacts in advance, which is the subject of the next section about strategic prevention steps.
How Do State Policy Changes Cause Family Care Program Pay Interruptions?
State policy changes—such as rate restructures, waiver reauthorizations, or adjustments to pass-through rules—alter the funding and payment mechanics for paid family care programs, and that shift can create temporary or permanent interruptions in caregiver compensation. Mechanically, a state change may require adjustments to billing codes, vendor contracts, or payment schedules; during the implementation window agencies often pause or reprocess existing payments to align with the new rules. A typical scenario is a state adopting a new minimum pass-through rate that requires administrative reconciliation; affected caregivers may see delayed checks while agencies update systems. These transitions also sometimes change who is eligible or how many hours are authorized, producing longer-term income reductions for caregivers until appeals or reauthorization restore prior levels.
When policy change is announced, caregivers should promptly verify program notices and engage enrollment specialists or advocates to understand transitional protections and timelines for implementation, which reduces the chance that a policy update will translate into an unexpected personal pay gap.
How Can Family Caregivers Prevent Payment Interruptions During Program Transitions?
Preventing payment interruptions starts with predictable administrative habits: proactive documentation, clear calendars for redetermination deadlines, and escalation plans for follow-up with state agencies and program administrators. A structured approach reduces the risk that a single missing form or missed deadline causes weeks without pay. The best prevention plans combine front-loaded preparation (organizing proof of income, ID, and care plans), scheduled reminders for key dates, and a short escalation playbook that identifies who to contact and when to escalate to supervisors or advocacy organizations.
Below is a step-by-step checklist caregivers can apply before and during transitions to minimize payment gaps.
Prepare and organize documentation: Gather beneficiary ID, proof of residency, income records, and current care plan in a single, labeled packet.
Track deadlines and set reminders: Note redetermination windows and set calendar alerts at 30, 14, and 7 days before due dates.
Submit early and confirm receipt: Send documents well before the deadline and obtain confirmation numbers or written receipts.
Maintain invoice and hour logs: Keep weekly hour tracking and invoices ready to resubmit if requested by the agency.
Escalate proactively: If confirmation isn’t received within normal processing time, contact state agency points of contact and request status updates.
This checklist translates into predictable outcomes: fewer suspended payments, faster resolution when holds occur, and clearer evidence if appeals are required.
Paid.care operationalizes several of these prevention tactics by offering eligibility checks, guided care coaching, and assistance facilitating weekly payments; their mobile app also supports eligibility checking, communication, care plan building, and hour tracking to help caregivers submit accurate documentation on time. Because Paid.care’s services are free for caregivers, using an eligibility assessment and coach can reduce administrative burden and help caregivers expedite applications or re-submissions during redetermination windows. Caregivers in service areas referenced for these operations—such as Indiana, Michigan, and Illinois—often use app-based hour tracking and coach guidance to shorten the time from submission to payment when agencies request additional information. The next section explains how minimum pass-through rates can further protect compensation.
What Strategies Ensure Continuous Paid Family Care Payments?
Continuous payments rely on both preventive administration and short-term cash-flow tactics that caregivers can apply when transitions are imminent or when a disruption has begun. Key strategies include preparing an emergency documentation packet, scheduling redundancy in communications (email plus tracked mail), and arranging short-term bridging funds or alternate paid work if permissible and safe for care obligations. Caregivers should also compile a clear escalation list—agency phone numbers, supervisor contacts, and local ombudsman resources—and keep copies of every submission to accelerate appeals or retroactive claims. When a payment pause occurs, immediate steps include contacting the program vendor, requesting status confirmation, and asking about interim payment options or emergency funds while the redetermination resolves.
A practical timeline approach helps: at 30 days before an expected review gather documents; at 14 days submit and confirm; at seven days follow up and verify receipt; and if payment pauses, begin escalation and appeal steps within the agency’s first 10 business days. These time-bound actions improve the probability that any gap will be measured in days rather than weeks.
How Do Minimum Pass-Through Rates Protect Caregiver Compensation?
Minimum pass-through rates are policy rules designed to ensure that increases to program funding or agency rates are actually passed on to caregivers rather than being absorbed by administrative intermediaries, and they protect caregiver compensation by setting a floor under paid rates during transitions. When states set or require pass-through minimums, agencies must preserve a baseline payment to caregivers even as vendor or administrative rates change; this buffer reduces the magnitude of income drops during restructures. Caregivers should learn whether their program includes such protections and, if not, pursue documentation or advocate for interim measures. When pass-through rules exist, dispute resolution typically requires showing the pre-change rate and the new vendor reconciliation; keeping clear records of prior payments and authorization letters therefore becomes essential to enforce minimums.
If pass-through minimums are unclear or not honored, caregivers can escalate via state Medicaid offices or advocate organizations to request enforcement or transitional relief, which is the next topic on eligibility and appeals.
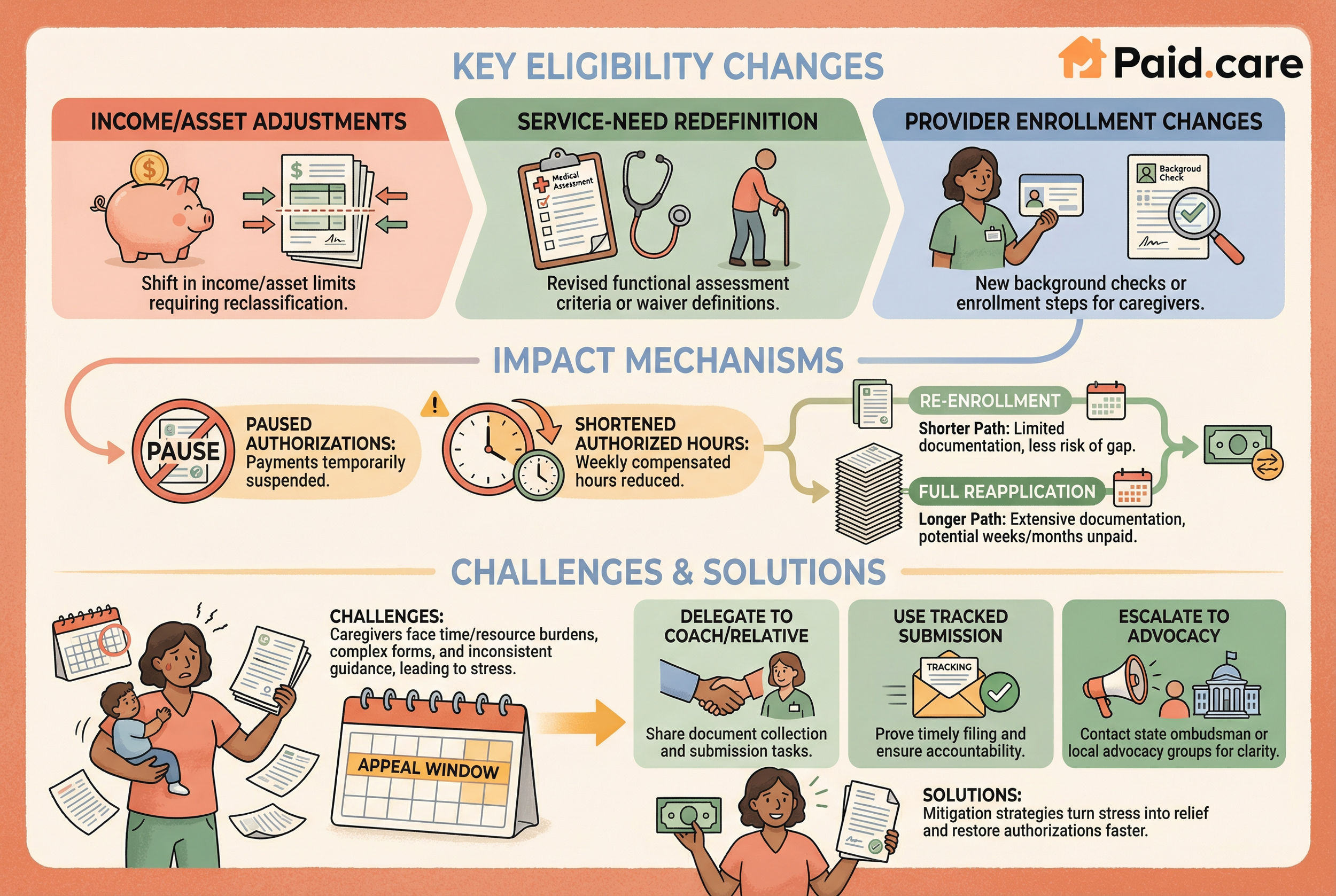
What Are the Key Eligibility Changes Affecting Paid Family Care Programs?
Eligibility changes that commonly affect paid family care programs include shifts in income or asset limits, redefinition of service-need criteria, and revised provider enrollment or background-check requirements; each type of change can convert an ongoing payment into a paused or terminated one. These eligibility shifts occur when states update waiver definitions, reinterpret functional need assessments, or align program rules with new federal guidance. The practical consequence for caregivers is that a beneficiary who previously qualified may require a new assessment or different documentation, prompting re-enrollment or full reapplication rather than a simple continuity update. Understanding which axis of eligibility is changing—financial, medical/functional, or provider enrollment—helps caregivers prioritize what evidence to gather and which procedural route to follow.
Below are concrete examples of how eligibility shifts change payment status and what caregivers should check to verify continued compensation.
Income or asset threshold adjustments: Changes can trigger reclassification from eligible to ineligible, requiring appeals or spend-down strategies.
Service-need redefinition: Modifying functional assessment criteria may reduce authorized hours or move a beneficiary between waiver types.
Provider enrollment changes: New background checks or enrollment steps for caregivers can temporarily suspend payments until credentials are updated.
How Do Eligibility Criteria Shifts Impact Family Caregiver Payment?
When eligibility criteria shift, the immediate mechanisms that alter caregiver payment include paused authorizations, shortened authorized hours, or full program exits pending reapplication, and each mechanism has distinct paperwork and timing requirements. For instance, a beneficiary moved to a program with stricter functional thresholds may see their authorized weekly hours cut, which directly reduces a caregiver’s compensated hours; in such cases caregivers often face a choice between unpaid care or seeking alternative paid shifts. Another scenario is administrative re-enrollment versus full reapplication—re-enrollment typically requires limited documentation and carries less risk of a long gap, whereas full reapplication can introduce weeks or months of unpaid status. Caregivers must therefore carefully confirm whether a change triggers simple re-certification or an entirely new approval pathway.
To manage these impacts, caregivers should prepare contingency documentation and understand appeal windows, because timely appeals or supplemental care plans can restore authorization faster than a new application.
What Are Common Challenges in Navigating Caregiver Eligibility Changes?
Caregivers face several operational and emotional challenges during eligibility transitions, including complex forms, inconsistent state guidance, and the time and resource burden of gathering documentation while providing care. The complexity is compounded when states interpret rules differently or when program staff turnover creates inconsistent instructions, leaving caregivers unsure which documents to prioritize. Time constraints are another major barrier: caregivers juggling direct care responsibilities may struggle to collect medical assessments, coordinate physician signatures, or attend required appointments. These burdens not only delay compliance but increase stress, which in turn can impair the caregiver’s ability to follow up rigorously on appeals or escalations.
Short mitigation tips include delegating document collection to a trusted relative or coach, using tracked submission methods to prove timely filing, and escalating inconsistencies to state ombudsman offices or local advocacy groups to obtain clarifying guidance quickly.
Which Alternative and Supplemental Programs Support Paid Family Caregivers?
Several program types can supplement or replace traditional paid family care arrangements, each with different structures that affect continuity and payment cadence; comparing them helps caregivers identify options to reduce income risk during transitions. The primary alternatives include Structured Family Caregiving (SFC) programs, Consumer Directed Personal Assistance (CDPAP) models, and Veteran-Directed Care programs. These programs differ in eligibility, authorization mechanics, typical payment cadence, and pass-through arrangements, and transitions between them can create gaps when enrollment or reauthorization is required.
Reviewing these differences helps caregivers weigh continuity versus flexibility when considering program switches, and the next subsections detail SFC specifics and the comparative dynamics between CDPAP and veteran-directed programs.
What Is the Structured Family Caregiving Program and Its Payment Gaps?
Structured Family Caregiving programs typically formalize an arrangement that pays family members for care under a specific waiver or state plan, and payment gaps can occur when program rules change or when beneficiaries transition between waivers. SFC programs usually rely on clear care plans and periodic reauthorizations; if a care plan is altered or a beneficiary is moved to another program type, the caregiver may face a pause while documentation and assessments are updated. Common payment-gap triggers include delayed authorizations for revised hours, changes to who qualifies as an authorized family caregiver, and administrative processing of new vendor enrollments. To reduce risk, caregivers should maintain updated care plans, secure physician documentation supporting the level of need, and proactively confirm reauthorization timelines with program staff.
These steps reduce the likelihood that administrative shifts in SFC will translate into prolonged unpaid care.
How Do Consumer Directed Personal Assistance and Veteran-Directed Care Programs Affect Pay Continuity?
CDPAP and veteran-directed care emphasize consumer choice and self-direction, which can help continuity because consumers control hiring and schedule decisions, but they also introduce administrative steps—such as caregiver enrollment, background checks, and vendor processing—that may create delays. In CDPAP models, the consumer typically needs to authorize the caregiver and confirm hours; any lag in enrollment or timekeeping verification can pause payment. Veteran-directed programs often involve coordination with veteran service coordinators and unique funding pools; transitions between VA funding and state programs may create reconciliation periods where payments are adjusted. Caregivers should check specific enrollment and verification timelines for these programs and plan to submit required documentation early to avoid service interruptions.
Understanding how self-direction shifts procedural responsibility to the consumer highlights why timely communication and documented approvals are central to pay continuity in these program types.
How Does Paid.care Help Family Caregivers Navigate Pay Gaps and Program Transitions?
Paid.care is a service dedicated to helping family caregivers get paid for providing in-home care to elderly or disabled loved ones, and its offerings map directly to many of the prevention and mitigation strategies described above. Paid.care provides eligibility checks, guided care coaching, and facilitation of weekly payments, which together reduce administrative friction and speed time-to-payment when program transitions occur. The service includes a mobile app for eligibility checks, communication, care plan building, and hour tracking; these features help caregivers assemble required documents, submit accurate timesheets, and maintain communication trails with agencies. Paid.care also pays competitive rates with weekly payments and may offer potential sign-on bonuses and benefits for qualified W2 caregivers, and importantly, Paid.care's services are free for caregivers, making it an accessible support option for those facing redetermination or policy changes.
Describing the operational flow clarifies how Paid.care reduces gap risk and accelerates recovery when interruptions occur.
How Does Paid.care Assist with Eligibility Assessment and Program Matching?
Paid.care assists caregivers through a stepwise workflow that begins with an eligibility check, proceeds to an assessment that identifies the best-fit program match, and then provides application support to reduce processing time and error. During the eligibility check, Paid.care screens for program fit and required documentation, helping caregivers prioritize what to submit to state agencies. The matching phase identifies suitable programs—such as family care waivers or consumer-directed options—and clarifies enrollment steps so caregivers avoid unnecessary reapplications. Finally, guided care coaching helps with document assembly, appeals when necessary, and coordination with payment vendors so caregivers can move from approval to compensation more quickly than handling the process alone.
This structured approach reduces paperwork errors, shortens administrative timelines, and improves the probability of continuous payment.
What Features of the Paid.care App Support Payment Tracking and Coaching?
Paid.care's mobile app centralizes key administrative functions that prevent and resolve pay gaps, including hour tracking, coach messaging, care plan builders, and payment visibility features that show pending and completed transfers. Hour tracking and verification let caregivers record work in real time and produce signed timesheets for state review, while coach communication channels allow direct guidance on document needs and escalation steps. The care plan builder captures authorized tasks and hours to align documentation with program requirements, and payment schedule visibility provides transparency on when weekly payments are processed or delayed. Using these features together creates a documented trail that agencies accept during reviews and appeals, which shortens resolution cycles and stabilizes caregiver cash flow.
This app-supported workflow complements the checklist and escalation practices discussed earlier and helps families keep records in audit-ready form.
What Are Frequently Asked Questions About Paid Family Care Pay Gaps and Transitions?
This section answers concise, high-value questions caregivers commonly have about avoiding payment gaps during program transitions, providing actionable steps and direct remedies that can be used immediately. The answers prioritize procedural clarity—what to file, when to call, and how to document—so caregivers can translate guidance into quick action. Each FAQ entry below is designed for immediate application and to be used in appeals or escalation calls.
How Can Caregivers Avoid Payment Gaps During Medicaid Redetermination?
Caregivers can avoid payment gaps by keeping beneficiary information current, submitting required documents early, and using support services when complexity increases. Specifically, update contact and address details immediately after any change, compile proof-of-income and residency documents before the redetermination window, and submit materials with confirmation receipts. If the process becomes contested, contact the program office and request supervisor review while retaining copies of every submission for appeal purposes. Using guided support from coaching services can also reduce errors that commonly cause suspensions.
These steps provide a practical short checklist caregivers can follow in the days and weeks leading up to redetermination.
What Causes Pay Interruptions and How Can They Be Resolved?
Pay interruptions commonly stem from administrative delays, eligibility changes, and payment processing errors, and each cause has a corresponding resolution pathway: follow up and request status updates for delays, file appeals with supporting evidence for eligibility changes, and contact payment vendors to correct processing errors. Administrative delays are often resolved by persistent follow-up and documented proof of timely submission; eligibility disputes typically require additional medical or financial evidence and may be resolved through formal appeal processes; and processing errors usually require vendor reconciliation plus proof of prior hours. Expected timelines vary, but proactive documentation and escalation typically shorten resolution from weeks to days.
Use the appropriate escalation path immediately—status follow-up for delays, appeals for eligibility, and vendor reconciliation for errors—to minimize unpaid periods.
Paid.care can assist caregivers in many of these steps by providing eligibility assessment, coaching, app-based hour tracking, and help facilitating weekly payments; caregivers seeking support to implement the preventive checklist and submit timely documentation may consider an eligibility check and guided enrollment support to reduce administrative burden and shorten time to payment. Paid.care’s services are presented as a practical operational tool to implement the strategies described above, especially for caregivers in service areas where app-based support and coach guidance are available. If you are navigating a program transition now, consider an eligibility check to confirm options and expedite any needed applications or appeals.
Would you like to find out exactly which Ohio program you qualify for and see your estimated pay rate? Visit Paid.Care today to start your free eligibility assessment.
FAQs
-
The Cause: This is the most common cause of pay gaps. Most programs automatically suspend payment the moment a client is admitted to a facility to prevent "double billing." However, they do not automatically restart when the client returns home.
The Fix: Contact your case manager 24 hours before discharge to trigger the "Return to Care" protocol. Ask specifically for the date and time your authorized hours resume. If you start working before that timestamp, those hours may be unpaid.
-
The Cause: Often, no. The "Old" waiver must close out its authorization before the "New" waiver can open yours. This administrative handshake can take weeks, leaving a period where no active authorization exists on file.
The Fix: Request a "Transition of Care" meeting with both the outgoing and incoming case managers present. Ask them to agree on a specific "cut-over date" where the old authorization ends at 11:59 PM and the new one begins at 12:00 AM to avoid a lapse.
-
The Cause: Most state and federal agencies do not offer interim loans or bridge pay for administrative delays. If your paperwork is stuck, you are generally expected to wait until approval is final.
The Fix: While direct bridge funding is rare, you can ask for "Presumptive Eligibility" (in some Medicaid programs) or "Expedited Processing" due to financial hardship. You must submit a written hardship letter stating that a delay in payment will force you to stop providing care.
-
The Cause: It depends entirely on the program's rules. Some programs allow "back-dating" to the date of application, while others strictly only pay from the date of approval.
The Fix: Never stop logging your hours. Even if you aren't being paid yet, submit your timesheets or keep a signed, daily log of care provided. If retroactive pay is approved later, you will need this simultaneous proof of work to claim the back pay.
-
The Cause: Usually, no. Medicaid and state-funded programs are often county-specific or state-specific. Moving across lines typically cancels your current authorization, requiring you to re-apply in the new location.
The Fix: Treat a move like a new job application. Apply to the agency in the new location months before you move. Ask if they accept "Reciprocity" (honoring the old assessment) to speed up the intake process, so you don't have to wait for a brand new medical evaluation.