Paid Family Care Pay Delays: Common Causes and How to Fix Them for Timely Caregiver Payments
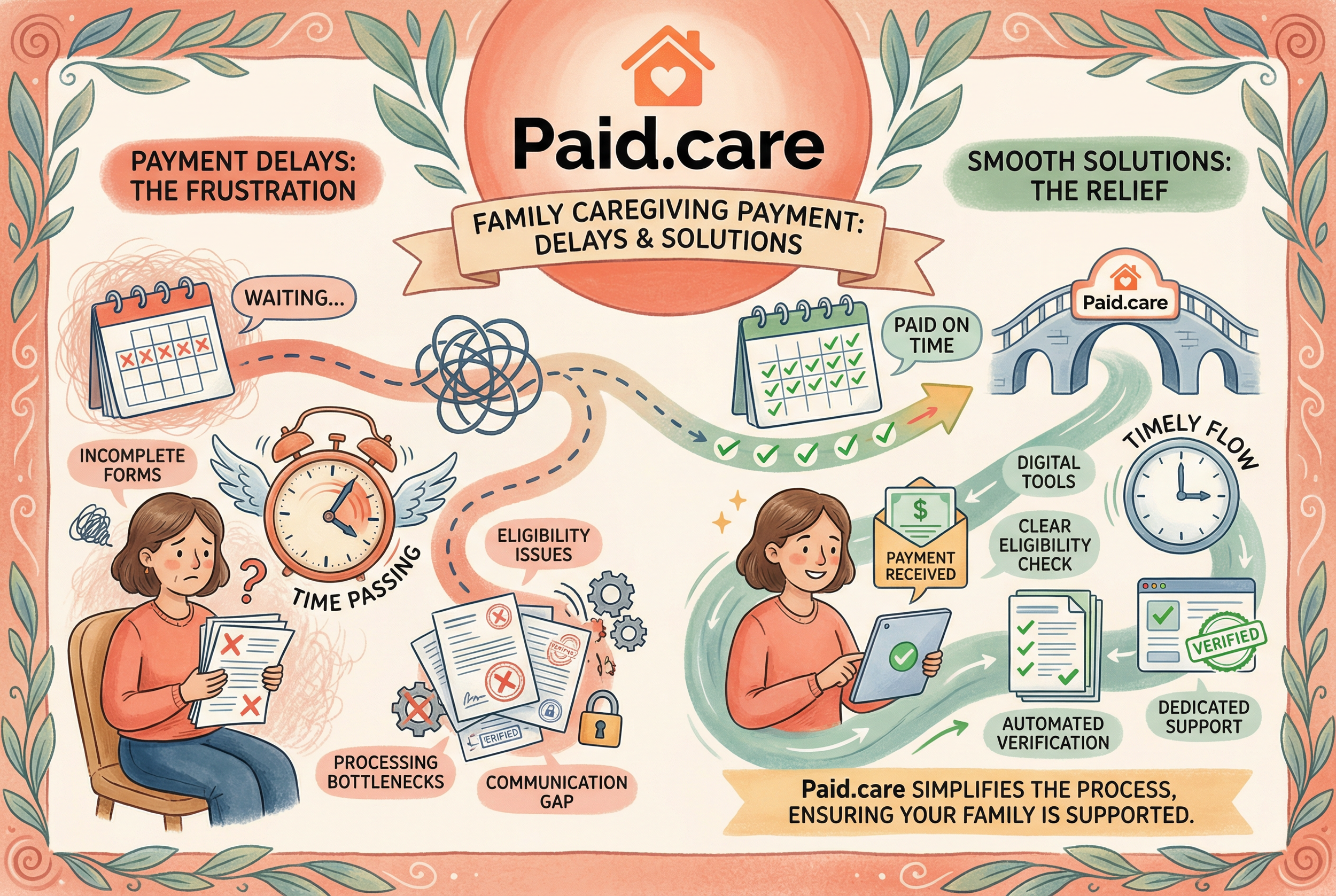
Delayed caregiver pay creates immediate financial strain and undermines the stability of home-based care arrangements, and many family caregivers find themselves chasing paperwork, eligibility checks, or bank confirmations instead of focusing on care.
This article explains what "paid family care pay delays" are, why they happen across programs like Medicaid, HCBS waivers, VA stipends, and Paid Family Leave, and delivers clear, prioritized fixes you can use right away. For caregivers who want hands-on help with eligibility checks, application assistance, documentation, or weekly pay facilitation, Paid.care can assist in many of the situations described; use their eligibility checker to see if you qualify. You'll get a mapped set of common root causes, program-specific troubleshooting for Indiana, Michigan, and Illinois, VA and paid leave workflows, and a step-by-step triage plan to minimize future holds. The guidance that follows blends practical checklists, sample scripts so you can diagnose delays faster and take the actions most likely to restore on-time payments.
What Are the Most Common Causes of Paid Family Care Payment Delays?
Payment delays for paid family care usually trace back to predictable root causes such as administrative errors, eligibility verification holds, missing documentation, program transitions, and banking or payment-rail failures. Each cause creates a different "hold state" in payment systems that prevents payroll runs or claim reimbursements until the issue is resolved. Understanding these mechanisms lets caregivers prioritize evidence collection and the correct office to contact, which shortens resolution times. The list below summarizes the most frequent causes and the immediate first action to take for each, helping caregivers form a quick triage.
Common causes and initial fixes:
Administrative errors: Verify payee name, SSN/TIN, and bank account details with the payroll or state vendor to correct mismatches.
Eligibility verification: Gather requested documents (ID, physician notes, care plans) and submit them promptly to the caseworker or eligibility team.
Missing or mismatched documentation: Reconcile signed care plans and timesheets with the payer’s required formats and resubmit with cover notes.
Program transitions: Track notices about vendor changes or waiver renewals and proactively confirm enrollment status with your caseworker.
Banking/payment rails: Confirm deposit attempts with your bank and request trace IDs from the payer to identify returned or delayed transfers.
This quick triage points to the next step: how specific administrative errors occur in practice and what a caregiver should check first when payments are late.
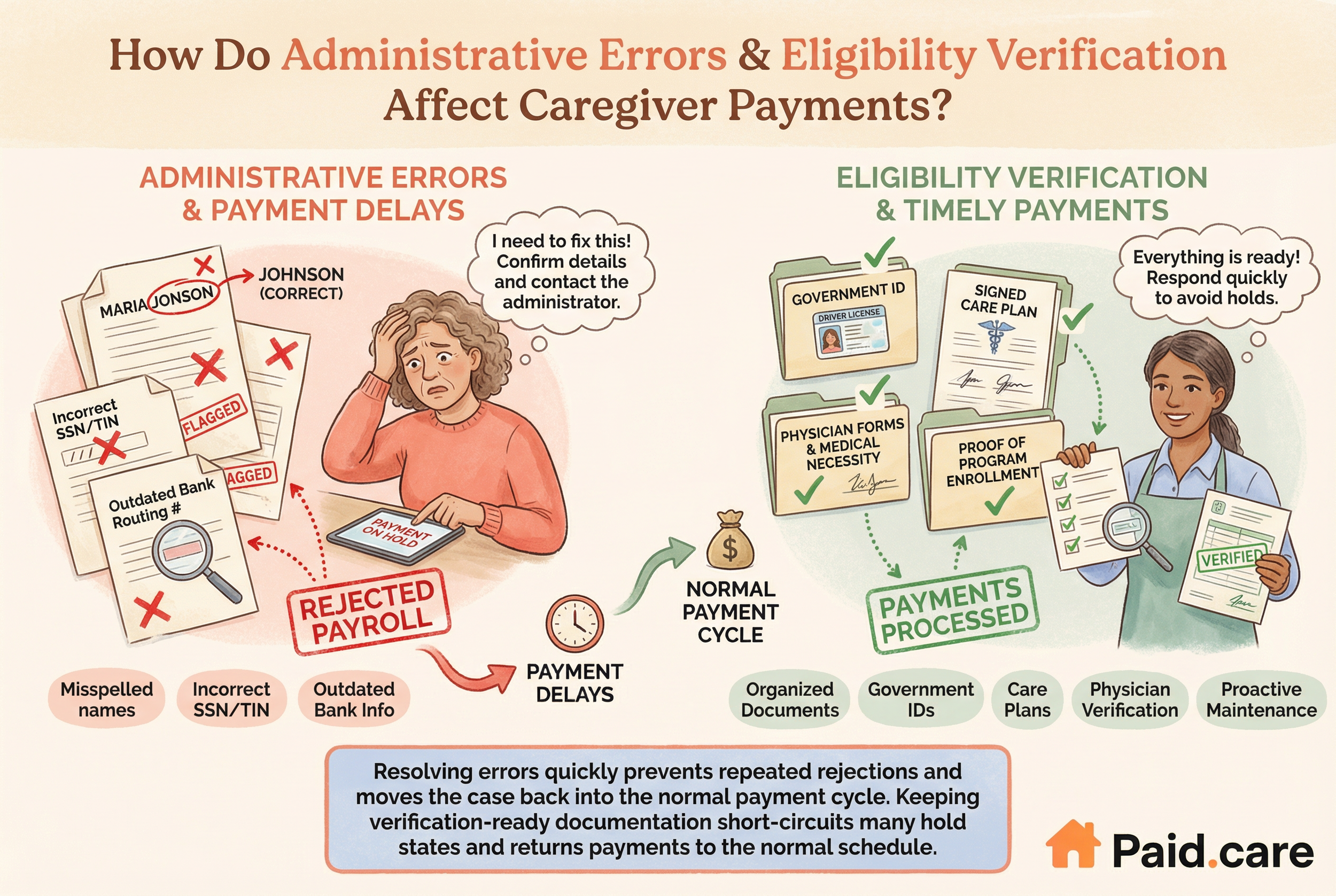
How Do Administrative Errors Lead to Caregiver Payment Delays?
Administrative errors often start with small data mismatches that cascade into rejected payroll runs or flagged claims, such as a misspelled name, incorrect SSN/TIN, or outdated bank routing numbers. These errors typically surface when payroll vendors validate records before issuing payments and will place accounts on hold until corrections are verified. Caregivers should run a simple verification checklist: confirm your name and SSN/TIN on file, verify bank account details on the vendor portal or with case management, and check that your timesheets match the payer’s expected format. When contacting administrators, use a concise script that states the discrepancy, the correct data, and asks for an estimated reprocessing date; this expedites correction because it gives the administrator the exact fields to update. Resolving administrative errors quickly prevents repeated rejections and moves the case back into the normal payment cycle.
Why Does Eligibility Verification Affect Timely Caregiver Payments?
Eligibility verification places payments into a controlled hold while agencies confirm that the care recipient and caregiver meet program rules, which can include residency, medical necessity, and caregiver enrollment requirements. Holds occur when supporting documents are incomplete or when the recipient’s status changes, triggering a new verification. Commonly requested documents include government ID, signed care plans, physician verification of need, and proof of program enrollment; missing any of these can create a gap that stops payment processing. To reduce verification delays, caregivers should proactively maintain a single folder of certified documents, respond quickly to requests, and ask the caseworker exactly which file type and signature format the agency requires. Keeping verification-ready documentation short-circuits many hold states and returns payments to the normal schedule.
How Do Medicaid and State Programs Impact Caregiver Payment Delays?
Medicaid-funded caregiver payments and state-administered programs have layered processing steps—eligibility, enrollment, timesheet verification, invoicing, and vendor payroll—that create multiple choke points where delays can occur. Each state handles claims and vendor relationships differently, so timetables and primary contacts vary, but the root mechanics are similar: a mismatch or missing step anywhere in the chain pauses downstream payments.
Caregivers in each state should use the table to match symptoms to the most effective first contact and documents to submit, which limits time spent cycling through generic agency channels and accelerates payment restoration.
What Medicaid Payment Issues Cause Delays in Indiana, Michigan, and Illinois?
In Indiana, administrative and reimbursement backlogs can create gaps when claims require manual review or when statewide vendor changes occur; caregivers should obtain claim IDs and follow up with the caseworker to request expedited processing. Michigan’s consumer-directed programs often face delays related to fiscal intermediary transitions or inconsistent timesheet submissions, so caregivers should confirm the accepted timesheet template and resubmit any mismatched records. Illinois may experience delays tied to HCBS waiver authorizations and invoicing cycles; caregivers should verify waiver approval dates and match invoice periods to the state’s billing window. Each of these examples points to a consistent remedy: gather the specific claim/authorization identifiers, submit the exact documentation the payer expects, and ask for a concrete reprocessing date.
How Do HCBS Waivers and Program Transitions Affect Payment Timing?
HCBS waivers and program transitions—such as moving to a new fiscal intermediary or shifting to a consolidated payment vendor—interrupt normal payment rails because the new system must ingest eligibility and historical billing data. During these transitions, some providers pause automated disbursements pending reconciliation, which delays caregiver payments until records align. Caregivers should monitor official notices about waiver status or vendor changes, proactively confirm their enrollment in the new system, and re-submit required forms if prompted. Maintaining an audit-ready record of previous approvals and timesheets shortens reconciliation time and reduces the chance that a historical omission will block payment under the new setup.
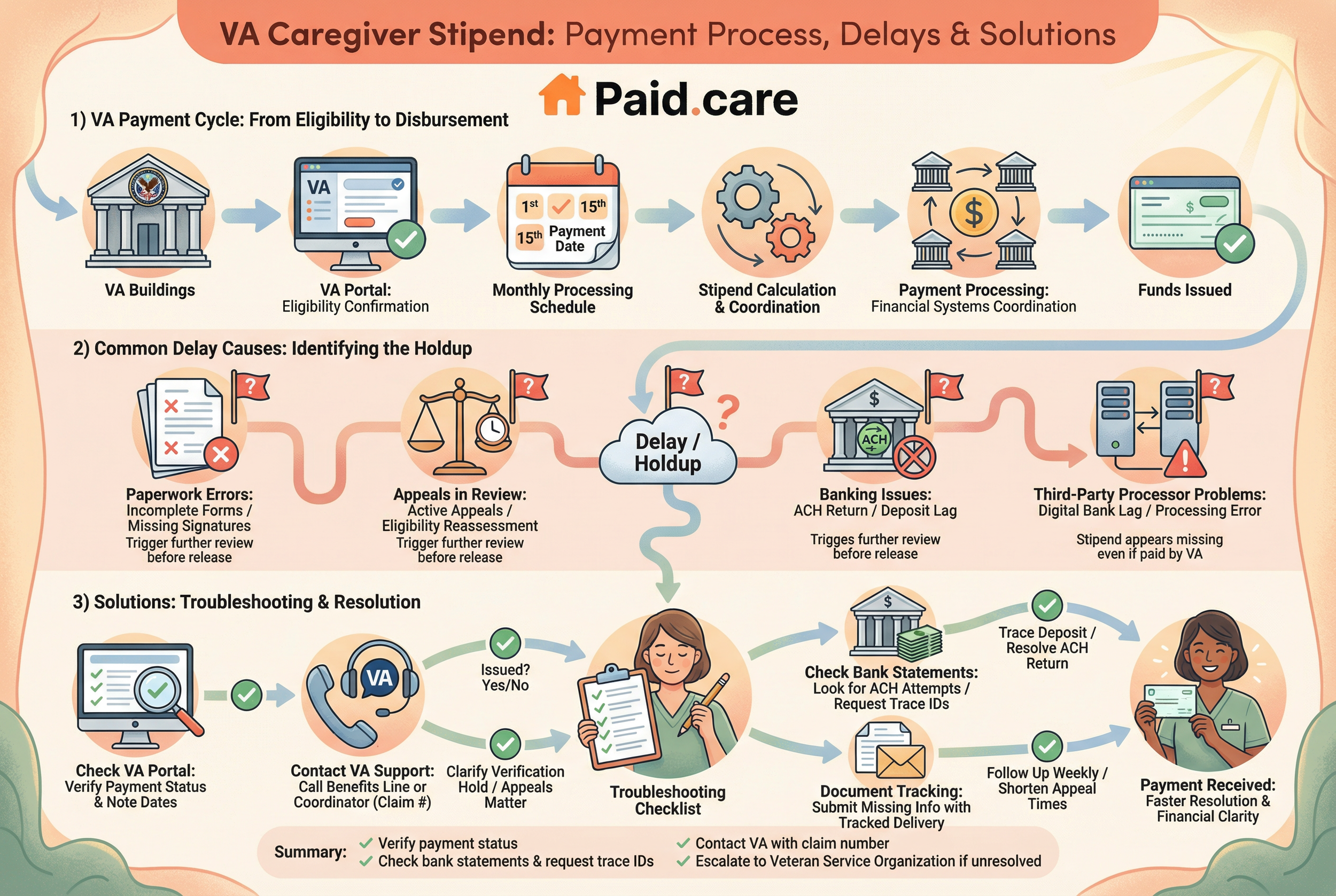
What Are the Causes and Solutions for VA Caregiver Stipend Payment Delays?
VA caregiver stipends follow defined processing cycles but can be delayed by paperwork errors, appeals or reviews, and banking or processor problems—especially when payment rails involve third-party or digital banks. The VA’s verification steps and appeals process can introduce weeks or months of delay if forms are incomplete or appeals are pending. Understanding the VA cycle and the role of banking partners helps caregivers know whether the delay sits with the VA, a payment processor, or the bank receiving the deposit. Begin by confirming the stipend status in the VA portal, then move to trace the deposit with your bank if VA records show payment issued; this isolates where to escalate next.
Key troubleshooting steps for VA stipends are summarized in the checklist below with escalation guidance.
Verify payment status on the VA portal and note payment dates.
Check bank statements for ACH attempts and request trace IDs from the VA if a payment shows as issued.
Contact the VA benefits line or caregiver support coordinator with claim numbers if paperwork or appeals are cited.
Why Are VA Caregiver Stipends Sometimes Delayed?
VA processing includes multiple layers—eligibility confirmation, stipend calculation, and coordination with financial systems—that can create delays when documentation changes or appeals are active. Another frequent source is banking or processor issues: an ACH return or a digital bank processing lag can make a stipend appear missing even after the VA marks it as paid. Paperwork problems often involve incomplete supporting medical documentation or missing signature pages, which trigger further review before funds release. When caregivers encounter delays, requesting a specific status code or payment trace from the VA clarifies whether the problem is a verification hold, an appeals matter, or a deposit issue, and that clarity guides the next corrective action.
How Can Caregivers Troubleshoot and Resolve VA Payment Problems?
Start by checking the VA portal to confirm whether the stipend shows as issued and record the payment reference or claim ID. If the portal indicates payment issued but nothing appears in your account, contact your bank with the VA payment reference to request a trace; the bank can often show whether an ACH was returned or delayed. If the VA shows a pending verification or appeal, obtain a written explanation of what documents are missing and submit those items with tracked delivery, then follow up weekly until the status changes. For unresolved cases, escalate to the caregiver support coordinator or use a veteran service organization as an advocate; documenting each contact and keeping copies of submissions shortens appeal times and supports faster resolution.
How Do Paid Family Leave Payment Problems Occur and How Can They Be Resolved?
Paid Family Leave (PFL) payments are delayed for three main administrative reasons: incomplete applications or verification, employer/HR submission bottlenecks, and state agency processing backlogs. Each pathway has a different immediate remedy—completing missing application fields, asking HR to re-submit claims promptly, or filing an inquiry with the state agency—so caregivers must triage based on where the stoppage occurs. Understanding the distinction between job-protected leave authorization and wage-replacement processing helps caregivers know whether to work with HR or the state agency first.
What Are Common Reasons for Paid Family Leave Payment Delays?
Common PFL issues include incomplete claim applications that lack required verification, employer-side delays when HR fails to forward documentation, and state agency processing capacity limits that extend normal timelines. Each reason produces distinct signals: a portal status of "incomplete" indicates missing fields, a payroll ledger that shows pending submission points to HR, and blanket delays or system notices often signal agency backlogs. Immediate fixes vary accordingly—completing and uploading missing documentation, escalating within HR, or filing a specific agency inquiry with proof of submission. Accurate diagnosis of where the hold exists lets caregivers apply the correct fix without wasting time on the wrong office.
What Steps Can Caregivers Take to Fix Paid Family Leave Payment Issues?
Verify your claim status in the agency portal and collect any required documents.
Contact your employer’s HR department to confirm whether they have submitted their portion and request re-submission if needed.
If neither step resolves the issue, file a formal inquiry or appeal with the state agency providing PFL, attaching proof of dates and signed documents.
What Practical Steps Can Caregivers Take to Fix and Prevent Payment Delays?
When a payment is late, follow a prioritized triage: (1) identify whether the hold is administrative, eligibility-related, or banking; (2) collect the exact documents or identifiers the payer requires; (3) contact the specific office (payroll vendor, caseworker, HR, or bank) with a clear script and request a reprocessing date; and (4) maintain an audit trail of every submission and phone call. Preventative habits include consistent, timestamped time tracking, keeping a verified document folder, and scheduling routine eligibility re-checks before renewal windows. These habits lower the probability of future delays by eliminating the common causes that create hold states.
Essential step-by-step numbered guide for triage and prevention:
Identify the hold type by checking portals, bank statements, and claim messages.
Gather exact documents and claim IDs the payer requests.
Use a clear contact script to request reprocessing and a concrete date.
Maintain digital copies and a contact log for all submissions and calls.
Adopt consistent time-tracking and proactive eligibility checks to avoid future holds.
After general actions, Paid.care can be a practical option: they offer eligibility checks, application assistance, free caregiver training and coaching, a mobile app for shift/time tracking and eligibility management, weekly payment facilitation, 24/7 support for eligibility/process guidance, assistance with Medicaid-funded payments, and financial coaching. Using a service that handles eligibility checks and weekly pay facilitation can reduce the administrative burden and lower the chance of recurrent delays.
Paid.care services:
Eligibility checks and application assistance to confirm enrollment and reduce verification holds.
Free caregiver training and coaching to ensure accurate documentation and proper timesheet practices.
Paid.care App for time tracking, care plan building, and storage of eligibility documents.
Weekly payment facilitation and 24/7 support to resolve issues quickly and maintain cash flow.
Financial coaching to help caregivers manage short-term gaps while disputes are resolved.
How Does Contacting Program Administrators Help Resolve Payment Delays?
Direct contact with program administrators often reveals the exact reason a payment is on hold because administrators can cite the claim ID, missing document, or rejection code blocking disbursement. When you call or email, have your case number, SSN/TIN, timesheet periods, and any prior correspondence ready; asking for the specific error code and an estimated reprocessing date produces actionable information. Use a short escalation script that requests supervisor review if initial contacts do not provide a timeline, and ask for an email confirmation of any promised updates. Persistent, documented follow-up converts ambiguous holds into fixable tasks and creates the record needed for appeals if the issue remains unresolved.
Why Is Accurate Documentation and Record Keeping Essential to Avoid Delays?
Accurate records—signed timesheets, physician notes, care plans, and proof of submission—are the evidence that moves claims from "under review" to "approved" and shortens dispute timelines. Maintaining a standardized naming and filing system, retaining documents for the agency-recommended retention window, and using digital timestamped uploads ensures you can respond immediately to verification requests. Digital tools for time tracking and document storage reduce human error and provide the exact artifacts payers often request when investigating delays. By preserving a single, organized source of truth, caregivers minimize friction during audits or appeals and significantly reduce payment downtime.
How Does Paid.care Support Caregivers in Overcoming Payment Delays?
Paid.care provides targeted services designed to reduce the administrative friction that causes caregiver payment delays and to streamline the path from eligibility to weekly pay. Their core offerings include eligibility checks and application assistance, free caregiver training and coaching, the Paid.care App for shift/time tracking and eligibility management, weekly payment facilitation, 24/7 support for eligibility and process guidance, assistance with Medicaid-funded payments, and financial coaching. Each feature maps to a specific delay cause—eligibility checks prevent verification holds, the App standardizes timesheets to avoid format rejections, and weekly pay facilitation closes gaps caused by payroll vendor timing.
Paid.care services in practical terms:
Eligibility checks and application assistance to confirm enrollment and reduce verification holds.
Free caregiver training and coaching to ensure accurate documentation and proper timesheet practices.
Paid.care App for time tracking, care plan building, and storage of eligibility documents.
Weekly payment facilitation and 24/7 support to resolve issues quickly and maintain cash flow.
Financial coaching to help caregivers manage short-term gaps while disputes are resolved.
What Services Does Paid.care Offer to Streamline Caregiver Payments?
Paid.care offers a set of services tailored to the exact delay causes described earlier: they perform eligibility checks and help with applications to avoid verification holds, provide free care coaching and training to improve documentation quality, and facilitate weekly payments to smooth cash flow during administrative processing. Their offering also includes 24/7 support for eligibility and process questions and assistance specifically designed to work with Medicaid-funded payment flows. These services reduce the time caregivers spend chasing paperwork and increase the likelihood of payments arriving on schedule.
How Can the Paid.care App Help Manage Eligibility and Ensure Timely Payments?
The Paid.care App centralizes shift and time tracking, care plan building, and eligibility documentation so timesheets and supporting files are formatted and stored consistently, reducing rejections and verification back-and-forth. App-based timestamps and stored documents provide the audit trail payers typically request, and integrated eligibility checks help detect potential enrollment gaps before they cause a hold. Getting started in the app involves confirming eligibility, setting up recurring shift logs, and uploading primary care documentation so the payer has immediate access; this preventative setup lowers the risk of delayed payments by addressing the most common administrative and verification causes.
FAQs
-
The Cause: Initial payments often undergo a rigorous "intake" verification process. The paying agency (such as Medicaid, the VA, or an insurance provider) must validate the care recipient's eligibility, confirm the caregiver's credentials/background check, and ensure all tax forms (like W-9s) are fully processed.
The Fix: Double-check that you have submitted all onboarding documents, no matter how small. Contact your case manager specifically to confirm your file is marked "complete" and ask for an estimated timeline for the initial deposit.
-
The Cause: Even timely submissions can be flagged for data errors. Common triggers include overlapping hours (claiming more than 24 hours in a day across multiple clients), missing digital signatures from the care recipient, or logging hours that exceed the authorized weekly maximum.
The Fix: Review your submitted timesheet for accuracy. If you find an error, submit a correction immediately. If the timesheet looks correct, call the payroll department to ask if a specific entry triggered a manual review or audit.
-
The Cause: Yes. If the care recipient is hospitalized, admitted to a skilled nursing facility, or enrolled in hospice, the funding source often pauses home care payments immediately to avoid "double billing" (paying for two services at the same time).
The Fix: Always report hospitalizations to your agency immediately. Do not log hours for days the client is in a facility. If the client has returned home, ensure the agency has processed their "return to care" paperwork so billing can resume.
-
The Cause: Yes, especially if you recently switched accounts or if there is a discrepancy in the routing number. Additionally, federal holidays can push direct deposit processing times back by one or two business days.
The Fix: Verify your direct deposit information with your payroll provider. If a holiday recently passed, wait 24 hours before worrying. If the delay persists, request a "trace number" from your payroll provider to give to your bank.
-
The Cause: This usually indicates a systemic issue rather than a one-time error. It could be an outdated authorization on file (where the approval for care has expired) or a recurring error in how you are coding specific tasks in the timesheet app.
The Fix: Schedule a meeting with your agency's billing coordinator. Ask if there is an issue with the "authorization period" for your client. Ensure that the care plan on file matches the hours you are actually working.