How to Appeal a Reduction in Paid Family Care Hours: A Complete Guide for Caregivers
Receiving a notice that your paid family care hours have been reduced can be frightening and confusing, but it does not have to be the end of services. This guide explains what a reduction means, why agencies like Medicaid, Paid Family and Medical Leave programs, and VA caregiver initiatives may cut hours, and what concrete steps caregivers can take to appeal those decisions. You will learn how to read a Notice of Adverse Action, what evidence strengthens an appeal, how to request aid continuing to maintain services while you appeal, and where to file a fair hearing or administrative review. The article walks through program-specific procedures, deadlines, and tactical templates to prepare medical records, care logs, and impact statements. Along the way, we’ll point to practical tools and supports—such as documentation management and caregiver coaching—that help organize evidence and preserve paid hours while your appeal proceeds.
What Are the Common Reasons for a Reduction in Paid Family Care Hours?
A reduction in paid family care hours typically stems from changes in assessed need, policy shifts, documentation gaps, or program-specific rules that govern benefits. Agencies reassess recipients periodically or after clinical updates, and when functional need appears to decline they may reduce hours to align with medical necessity criteria. Funding or policy changes at the state or program level can also force recalculations of authorized hours, while errors or missing documents sometimes produce adverse determinations that are reversible with better evidence. Understanding these common causes helps caregivers anticipate the documentation and procedural responses required to challenge a reduction effectively.
Why Do Medicaid and Other Programs Reduce Care Hours?
Medicaid and similar programs reduce care hours when assessments conclude that the recipient no longer meets the same level of functional need required for previous authorizations; the mechanism is a medical necessity evaluation that links clinical findings to service hours. Managed Long Term Care plans and state HCBS programs use standardized assessments that translate ADL/IADL limitations into hour allocations, so changes in mobility, cognition, or prescription regimens often trigger hour adjustments. Administrative triggers—such as periodic reassessments, missing recertification paperwork, or updated provider notes—also lead to reductions, which vary by state and program rules. Because program criteria differ, it’s important to check the specific Medicaid or managed care guidance in your state to understand what evidence will counter a proposed reduction.
How Does a Notice of Adverse Action Affect Caregivers?
A Notice of Adverse Action is a formal document explaining the agency’s decision to reduce or stop services and it typically sets an official deadline for appeal or request for reconsideration, creating immediate obligations for caregivers. The notice usually lists the reason for the change, the effective date, the date the notice was mailed, and the procedural steps to appeal; missing the stated deadline can forfeit appeal rights in many programs.
Upon receipt, caregivers should document the notice date, preserve copies, and immediately begin gathering medical evidence and care logs that demonstrate ongoing need. Acting quickly after receiving a notice preserves both legal options—like aid continuing in some programs—and practical leverage to present timely, persuasive documentation.
Common administrative reasons for reductions include reassessment results, missing documentation, policy changes, and clerical errors.
Immediate actions after a notice are to verify the effective and mail dates, note the appeal deadline, and request aid continuing if available.
Understanding the specific contents of the notice helps determine whether to request expedited review, submit new evidence, or seek legal help.
These steps prepare caregivers for the next topics: rights and appeal options that protect recipients during the review process.
What Are Your Rights and Options When Care Hours Are Reduced?
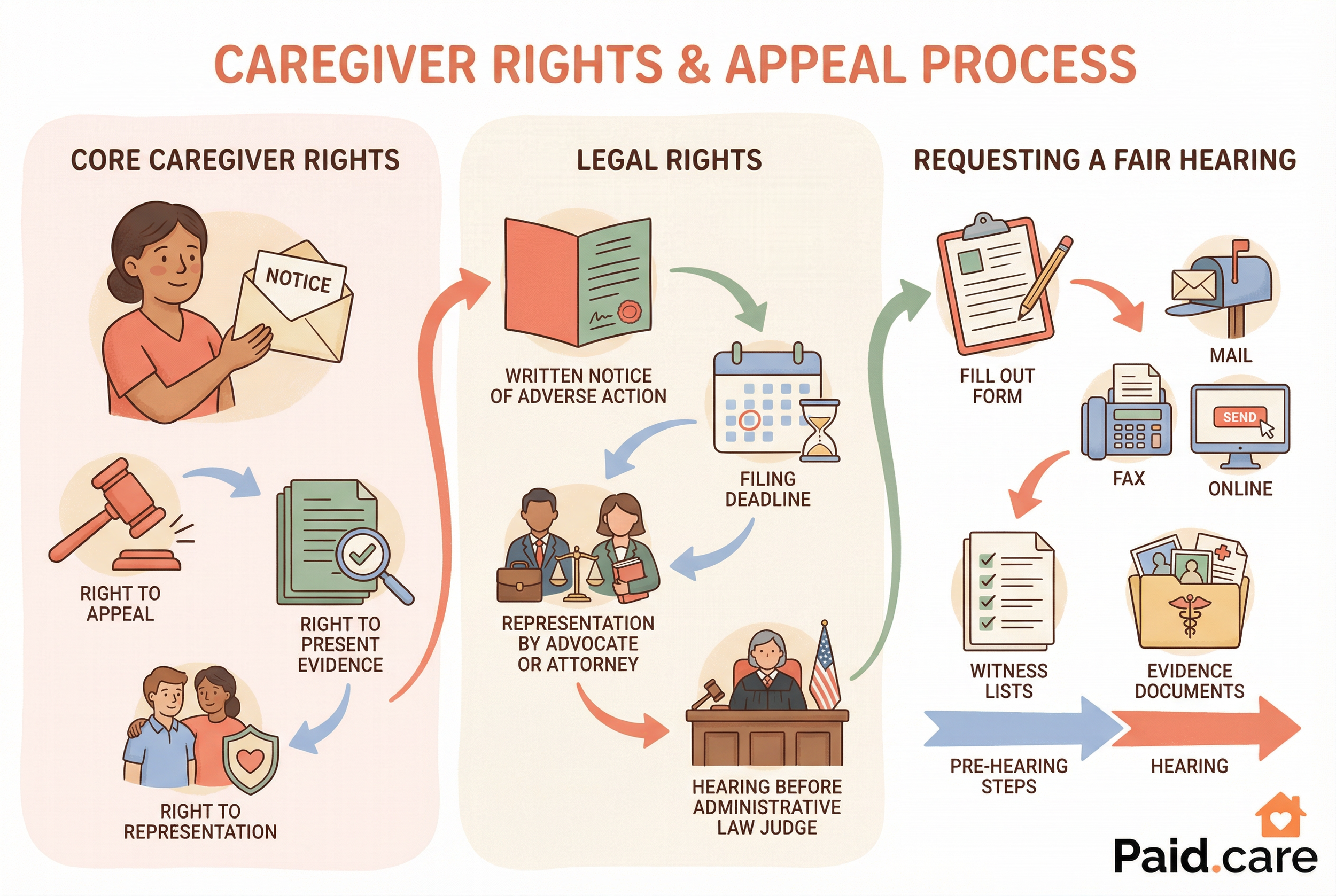
Caregivers and recipients generally have core rights that include timely written notice of reductions, the right to appeal, the ability to present evidence, and the option to request representation or legal aid when pursuing administrative reviews. These protections are rooted in due process and program regulations across Medicaid, PFML, and VA caregiver support programs, which typically require agencies to provide procedural information with their adverse notices. Options after a reduction include requesting reconsideration, filing a formal appeal or fair hearing, submitting supplemental documentation to correct record errors, and seeking advocacy or legal representation. Understanding these rights helps caregivers choose the best procedural route—reconsideration for quick fixes or formal hearings for disputes needing adjudication.
What Legal Rights Do Caregivers Have to Appeal Reductions?
Legal rights commonly available across programs include the right to written notice explaining the adverse action, the right to file an appeal within a prescribed deadline, and the right to be represented or assisted by an advocate or attorney during hearings. Administrative rules also typically permit submission of new or corrected evidence and the opportunity to question or cross-examine witnesses at a hearing before an Administrative Law Judge or equivalent. Remedies vary and can include restoration of hours, partial restoration, or a written explanation sustaining the reduction, so caregivers should document the basis for their challenge and consider reaching out to legal aid, elder law attorneys, or advocacy organizations that specialize in program appeals. These legal options lead directly to practical steps for requesting hearings and preparing evidence.
How Can You Request a Fair Hearing or Administrative Review?
Requesting a fair hearing usually requires filing a written appeal form or letter with the agency listed on the Notice of Adverse Action and doing so within the stated deadline; many agencies accept mail, fax, or online submissions where available. The request should include identifying information, a clear statement that you are appealing the reduction, the date of the notice, and any immediate request for aid continuing if that applies to your program; attach any evidence you already have and indicate whether you plan to have representation or witnesses. After filing, expect a timeline that can include pre-hearing conferences, document exchange, and a hearing before an Administrative Law Judge or hearing officer, and prepare testimony, witness lists, and exhibits accordingly. Preparing procedural documents and witness statements early increases your chance of a favorable outcome and helps preserve services while the appeal is pending.
How Do You File an Appeal for Reduced Paid Family Care Hours?
Filing an appeal for reduced paid family care hours follows program-specific steps but shares foundational actions: review the notice, note the deadline, file a timely appeal, submit supporting evidence, and request aid continuing where applicable. Taking these steps quickly preserves rights and creates a clear record for the adjudicator. Below is a concise checklist designed for featured-snippet clarity that caregivers can follow immediately after receiving an adverse notice.
Review the Notice: Confirm the effective date, reason for reduction, and appeal deadline listed on the notice.
Note Deadlines: Calculate the exact appeal deadline from the notice mail or receipt date and mark it in writing.
File the Appeal: Submit the prescribed appeal form or written request to the agency before the deadline, using the method accepted in your program.
Request Aid Continuing: When eligible, request continuation of previously authorized services pending appeal to prevent loss of care.
Gather Evidence: Assemble medical records, physician statements, detailed care logs, and impact statements to support the appeal.
Prepare for Hearing: If a hearing is scheduled, organize exhibits, witness testimony, and a clear timeline of events for submission.
Seek Help: Contact legal aid, advocacy groups, or representatives experienced in Medicaid, PFML, or VA appeals for assistance.
This checklist leads into program-specific filing details, which are summarized below to help you identify the right forms and contacts.
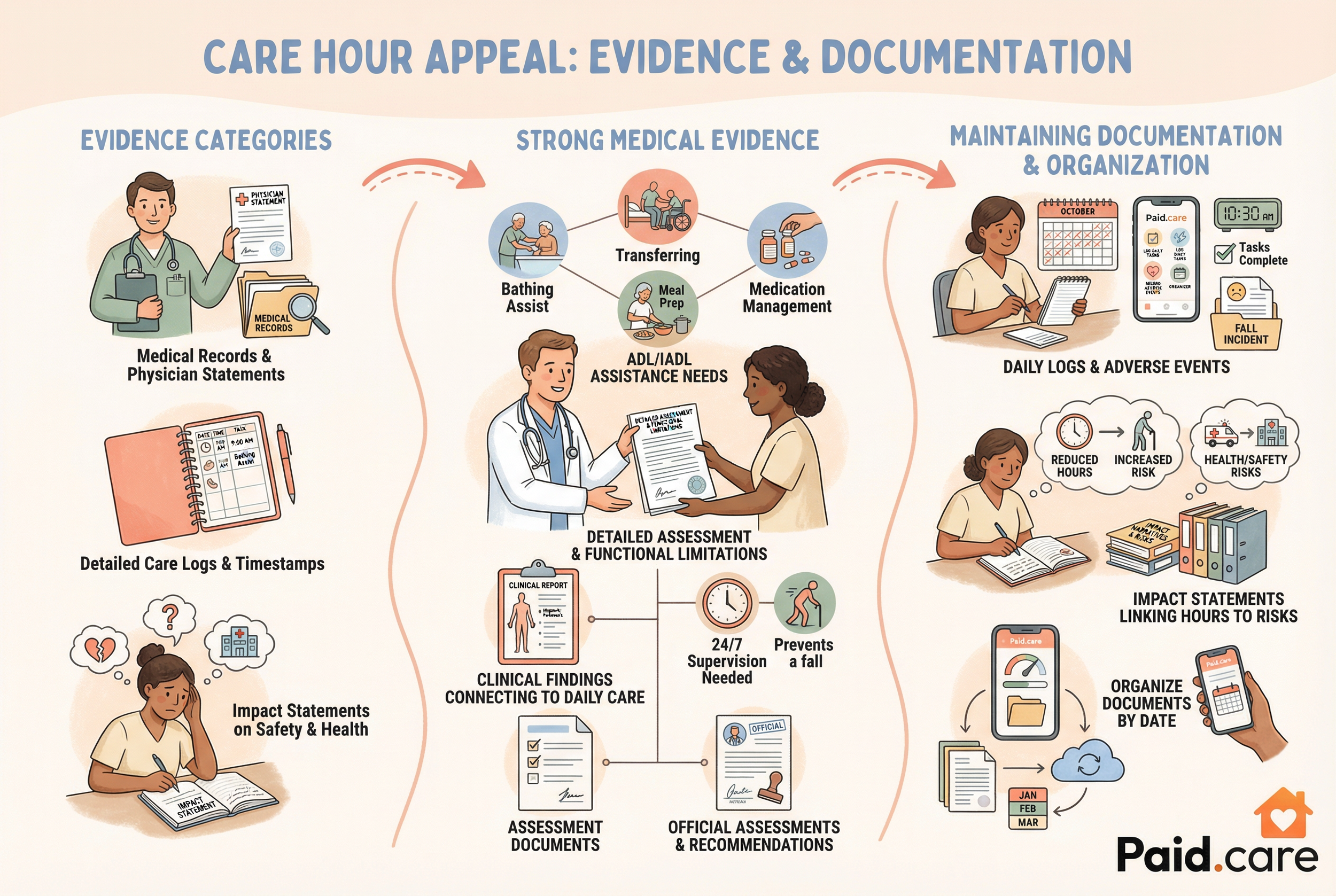
What Evidence and Documentation Are Needed to Support Your Appeal?
Successful appeals rely on clear, contemporaneous evidence that links the recipient’s functional limitations to the hours previously authorized. Evidence categories include physician statements that describe ADL/IADL assistance needs, complete medical records and therapy notes, hospital discharge summaries, detailed care logs with timestamps, medication lists, and impact statements that explain health or safety risks when hours are reduced. Presenting organized documentation that shows how daily tasks require assistance—rather than only clinical diagnoses—strengthens the case because many programs base hours on functional need. Below is a practical list of essential evidence types and why they matter to help you prioritize what to collect and submit.
Medical records and physician statements that document ongoing functional limitations and required assistance.
Detailed care logs recording tasks performed, time spent, and specific observations about the recipient’s condition.
Impact statements from caregivers and recipients describing worsened safety, missed treatments, or increased emergency visits.
Which Medical Records and Physician Statements Strengthen Your Case?
Physician statements that explicitly describe functional limitations—such as the need for assistance with bathing, transferring, meal preparation, medication administration, or supervision—are particularly persuasive because they connect clinical findings to daily care needs. Clinicians should include objective assessment results, brief descriptions of observed limitations, frequency and duration of required assistance, and an opinion on why previously authorized hours remain necessary. To obtain these records, request succinct, dated letters or standardized functional assessments from treating providers, and ask medical records departments for copies of recent notes, therapy summaries, and hospital discharge paperwork. When clinicians provide clear, function-focused language, adjudicators can more readily map that evidence to the hour allocation criteria used by programs.
How to Maintain Care Logs and Impact Statements for Appeals?
Consistent, detailed care logs and impact statements transform anecdotal observations into admissible evidence that adjudicators rely on to measure real-world need. A care log should include date, start and end times for each task, task description (e.g., assistance with dressing, transfers, medication), and any adverse events or safety concerns observed; logs with timestamps and signatures increase credibility. Impact statements should be concise narratives that explain how reduced hours affect health, safety, and daily functioning—linking examples to dates, missed care, falls, or hospital visits whenever possible. Keep copies organized by date and create a simple index of documents for submission; this organization helps presenters during hearings and makes it easier for hearing officers to follow your argument.
Paid.care’s app and documentation tools provide practical ways to organize medical records, care logs, and impact statements for appeals. Paid.care helps family caregivers get paid for in-home care by facilitating qualification for state and government programs (including Medicaid, HCBS, consumer-directed programs, veteran-directed care, and paid family leave). Paid.care offers eligibility checks, caregiver coaching, training, certifications, weekly payments, a proprietary mobile app for managing care and communicating with experts, free care coaching, 24/7 support, competitive pay rates (example: over $250/day in Indiana), and a $1,000 sign-on bonus for qualified W2 caregivers. Using structured digital logs and secure document uploads can shorten the time to compile bundles of evidence for filing, and coaching helps translate daily observations into effective impact statements. These tools are supplemental to the legal and procedural steps already described, and they are intended to make evidence management and communication with experts more efficient during an appeal.
How Can You Maintain Benefits During the Appeal Process?
Maintaining benefits during an appeal often depends on program rules for aid continuing or service continuation pending appeal; when available, aid continuing preserves previously authorized services while the case is adjudicated. Eligibility for aid continuing typically requires filing a timely appeal and specifically requesting continuation on or before the appeal deadline, and sometimes the request must be made in writing or via a designated form. Practical steps to protect services include submitting a written aid continuing request with the appeal, attaching supporting evidence that shows urgency or risk, and asking for expedited review if health or safety is at stake. Acting promptly to request continuation reduces the likelihood of immediate service gaps while you prepare a full case for the hearing.
What Is Aid Continuing and How Do You Request It?
Aid Continuing is a procedural protection that keeps previously authorized services in place while an administrative appeal is pending, ensuring recipients are not left without care during the review period. To request aid continuing, file your appeal within the deadline and include a written request for continuation—clearly stating that you want formerly authorized services to continue pending the appeal decision—and attach any relevant supporting documents that show ongoing need. Some programs require a specific checkbox or form language; when in doubt, include a clear statement in your appeal letter and make sure to keep proof of submission. Documenting your request and following up with the agency preserves your right to continued services and strengthens your procedural record.
What Are the Critical Deadlines to Protect Your Paid Care Hours?
Deadlines to appeal or request aid continuing differ by program and sometimes by state; common windows include short ranges like 10 days for employer or insurer notices, 30 days for many state-administered appeals, and up to 60 or 90 days for certain federal or VA processes. The official deadline shown on your Notice of Adverse Action controls, and calculating the deadline typically begins from the mailing or receipt date indicated on that notice. Missing the deadline often waives appeal rights except in narrow circumstances like good-cause extensions, so immediate action—documenting the notice, filing an appeal, and requesting aid continuing where allowed—is essential. If you are unsure, treat the shortest possible deadline as binding until you confirm otherwise and seek assistance from advocates or legal resources to preserve rights.
Typical deadline examples by program: 10–30 days for PFML or insurer notices, 30–90 days for Medicaid fair hearings, 60 days common in VA contexts.
Always calculate deadlines from the notice’s mail or receipt date and note whether “postmark” vs. “received” rules apply.
If a deadline is missed, consider filing a good-cause extension request immediately and document reasons why the appeal was late.
These deadline tactics feed directly into preparation for hearings and evidence submission described earlier.
How Can Paid.care Support You Through the Appeal Process?
Paid.care provides a range of practical supports designed to help caregivers manage eligibility and documentation during appeals, and to stabilize finances while appeals proceed. Paid.care helps family caregivers get paid for in-home care by facilitating qualification for state and government programs (including Medicaid, HCBS, consumer-directed programs, veteran-directed care, and paid family leave). Paid.care offers eligibility checks, caregiver coaching, training, certifications, weekly payments, a proprietary mobile app for managing care and communicating with experts, free care coaching, 24/7 support, competitive pay rates (example: over $250/day in Indiana), and a $1,000 sign-on bonus for qualified W2 caregivers. These services aim to reduce administrative burden, organize evidence for appeals, and provide short-term financial stability through weekly payments while you pursue restoration of hours.
What Coaching and Resources Does Paid.care Offer for Caregivers Facing Reductions?
Paid.care’s coaching services focus on documentation assistance, appeal preparation, and connecting caregivers to state-specific resources or advocacy networks that help argue for restored hours. Coaches assist with organizing medical records, drafting impact statements, and preparing care logs in formats suitable for submission to agencies or hearing officers. Financial coaching and weekly payment support help caregivers maintain household stability while appeals proceed, and training and certifications strengthen caregiver credentials that can be relevant to program eligibility. Paid.care also offers free care coaching and 24/7 support to answer questions during the appeal timeline, which can help caregivers prioritize evidence collection and follow procedural deadlines under pressure.
How Does the Paid.care App Help Track Hours and Prepare Appeal Documentation?
Paid.care’s proprietary mobile app is designed to capture time-stamped care logs, task descriptions, and secure document uploads that can be exported as audit-ready reports for appeals and hearings. The app enables caregivers to record start and end times, attach notes about safety events or missed treatments, and store physician statements or discharge summaries in a central location for easy retrieval. Exportable logs and PDF-ready documentation streamline submission to agencies and hearing officers, while communication features let caregivers consult coaches and experts about preparing concise evidence bundles. Using structured exports from the app reduces manual compilation time and presents a consistent, chronological record that adjudicators can follow during review.
App features include time-stamped task logs, document storage and export, and communication with coaches and experts.
Exported reports can be used as exhibits in hearings and are formatted to match common agency expectations.
Secure storage and coach support help ensure that evidence is admissible, organized, and persuasive.
This ends the set of required sections and practical guidance about appeals, evidence, aid continuing, and program-specific processes. For caregivers facing reduced hours, the next step is to file the appeal, gather the prioritized evidence described above, request aid continuing when eligible, and consider Paid.care’s eligibility checks and coaching supports to streamline documentation and maintain stability during the appeal.
Don't leave money on the table or struggle through the application process alone.
FAQs
-
The Strategy: You must request "Aid Paid Pending" (sometimes called "benefits continuing"). In most Medicaid and state programs, if you file your appeal within 10 days of receiving the Notice of Action (the letter informing you of the cut), your hours will remain at their current level until the hearing decision is made.
The Risk: If you lose the appeal, some states may require you to pay back the "extra" money paid out during the appeal period. However, many caregivers find this risk worth taking to ensure continuity of care.
-
The Cause: Hours are rarely cut because a diagnosis changed; they are cut because the "functional assessment" changed. A caseworker may have observed the recipient doing a task independently (like feeding themselves) that they previously needed help with. Alternatively, a "natural support" (like a spouse retiring and being home more) may have been identified, reducing the hours the state deems "medically necessary" for a paid provider.
The Fix: Request a copy of the specific assessment form (e.g., the SOC 293 in California or the comprehensive assessment in your state). Compare it line-by-line with the previous year's assessment to find exactly which task was scored lower.
-
The Standard: A doctor’s note saying "Patient needs care" is not enough. You need quantitative evidence.
The Fix: Create a "24-Hour Care Log" for three days leading up to the hearing. Document every single intervention: "10:00 AM - Assisted to toilet (15 mins)," "10:45 AM - Redirection due to dementia wandering (10 mins)." Combine this with a letter from the doctor that specifically refutes the state's finding (e.g., "Contrary to the assessment, the patient cannot transfer safely without human assistance due to severe neuropathy").
-
The Process: It is generally much less formal. It is an administrative hearing, usually held in a small conference room or over the phone with an Administrative Law Judge (ALJ). You do not need a lawyer, though you can bring an advocate.
The Strategy: Speak clearly and stick to the facts. When the county/agency representative presents their reason for the cut, wait for your turn and then present your "Care Log" and medical letters as direct rebuttal evidence. Focus on safety risks—explain what would happen to the patient's health if these hours remain cut.
-
The Cause: Programs often reduce hours if the caregiver lives with the recipient, assuming that "general household chores" (like cleaning common areas) would be done anyway.
The Fix: Yes, you can appeal this, but you must prove that the tasks are exclusively for the recipient. For example, if you are cleaning the recipient's bedroom or preparing a special medically required diet that no one else eats, those tasks should not be prorated or reduced just because you live there.