Michigan Medicaid Income Limits 2025: Eligibility and Payment Guide for Family Caregivers
Michigan Medicaid provides health coverage and long-term services that determine eligibility based on income, assets, and program rules, and 2025 income limits are central to whether a care recipient — and by extension their family caregiver — can participate in payment programs. This guide explains how Michigan uses the Federal Poverty Level (FPL) and MAGI-based calculations to set income thresholds, how different programs such as the Healthy Michigan Plan, Home Help, and HCBS waivers interact with caregiver payment, and what steps families must take to apply. Many family caregivers need clarity on which income tests and asset rules matter, how spend-down works when income is too high, and how consumer-directed models enable family members to be paid. The article maps income tables, asset comparisons, program pathways, step-by-step application instructions, and practical preparation checklists so caregivers can act with confidence. Throughout, readers will find quick-reference tables, actionable lists, and a brief description of how Paid.care supports caregivers ready to confirm eligibility and organize payments under Michigan Medicaid.
What Are the Michigan Medicaid Income Limits for 2025?
Michigan determines Medicaid eligibility using income thresholds tied to the Federal Poverty Level (FPL) and, for many adults, Modified Adjusted Gross Income (MAGI) rules; these thresholds differ by program and household size. Income limits control whether an applicant qualifies for coverage and for which program they qualify, which in turn affects if a family caregiver can be paid. Below is a focused table showing common program thresholds expressed as percent of FPL with example annual and monthly amounts for 2025; these figures provide a practical starting point to gauge eligibility for single adults and small families. Understanding where an applicant falls relative to these thresholds helps families select the right Medicaid pathway and anticipate whether spend-down or asset rules will apply. The next subsection explains how FPL percentages are converted into concrete income amounts for application and budgeting purposes.
How Is the Federal Poverty Level Used to Determine Income Limits?
The Federal Poverty Level is a yearly income standard used to calculate eligibility for many means-tested programs; states and programs apply a percentage of FPL to set income limits for 2025. MAGI-based programs compare a household’s Modified Adjusted Gross Income to a percent of FPL (for example, 138% FPL for many expansion populations) and convert annual thresholds to monthly limits by dividing by 12. This conversion makes it practical to evaluate pay stubs or monthly benefit estimates during application and to determine whether a spend-down is necessary when income exceeds the limit. Programs that are non-MAGI use different counting rules and may apply strict asset tests in addition to income thresholds. Understanding the FPL method helps applicants know which program’s rules apply and which documents to prepare for MI Bridges or MDHHS assessment.
Which Michigan Medicaid Programs Support Family Caregivers with Payment?
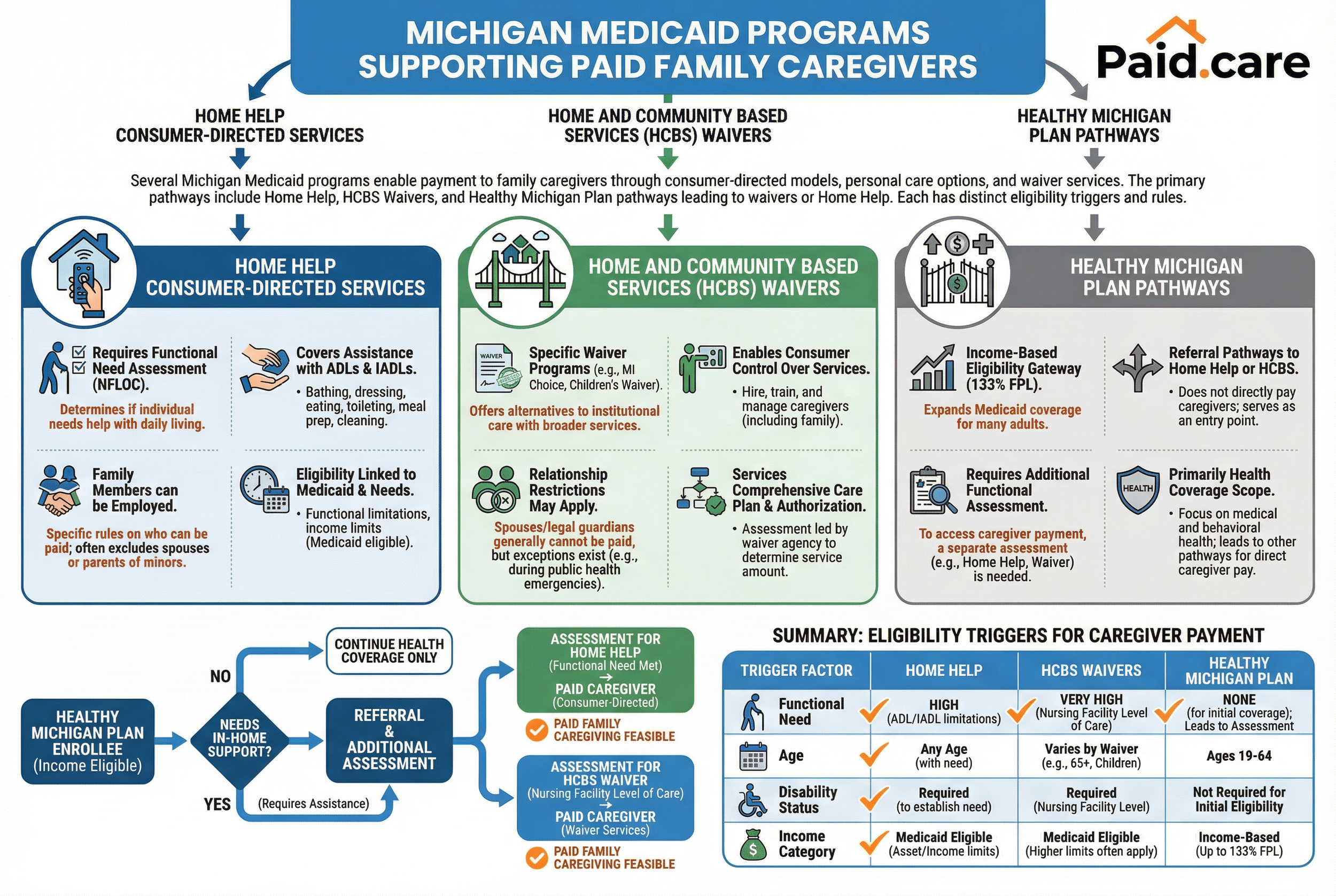
Several Michigan Medicaid programs enable payment to family caregivers through consumer-directed models, personal care options, and waiver services; mapping programs to caregiver payment routes helps families identify where paid caregiving is feasible. The primary program types that support caregiver payment include Home Help consumer-directed services, Home and Community Based Services (HCBS) waivers that allow consumer direction, and coverage pathways under the Healthy Michigan Plan when paired with waiver or home help benefits. Each program has distinct eligibility triggers — such as functional need, age, disability status, or income category — and different rules about who may be employed or paid as a caregiver. The table below compares these programs and indicates how they enable caregiver payment in practice. After the table, the Healthy Michigan Plan subsection clarifies where it broadly fits in this landscape.
How Does the Healthy Michigan Plan Affect Caregiver Eligibility?
The Healthy Michigan Plan expands Medicaid coverage for many adults under income-based eligibility and can be an entry point to services that lead to caregiver payment when paired with waiver or home help assessments. In some cases a Healthy Michigan Plan enrollee who needs in-home supports will be referred to HCBS or Home Help evaluations that permit consumer-directed hiring of family caregivers. However, the Healthy Michigan Plan on its own is primarily health coverage and does not always directly authorize paid caregiving without an additional assessment that documents functional need. Families should verify coverage pathways during the assessment step to determine whether a waiver or Home Help enrollment will follow from Healthy Michigan Plan eligibility.
What Are the Asset Limits and Spend-Down Rules for Michigan Medicaid?
Certain Michigan Medicaid programs apply asset limits while others focus solely on income, and spend-down is the process used when income exceeds program limits but assets disqualify the person from meeting eligibility without allowable medical deductions. Programs for aged, blind, or disabled beneficiaries typically impose asset tests with specific thresholds and count certain resources while exempting others, whereas MAGI-based programs usually do not apply asset limits. Spend-down works by subtracting allowable medical expenses from income to reach an eligibility level; a worked example clarifies how a family might qualify temporarily while arranging long-term eligibility. The table below summarizes which programs have asset limits, typical thresholds, and examples of counted versus exempt assets so families can plan documentation and financial strategies.
Which Assets Are Counted or Exempted in Medicaid Eligibility?
When asset tests apply, counted assets commonly include bank savings, investments, and non-exempt vehicles or property, while typical exemptions include the applicant’s primary residence (with equity limits in some cases), one vehicle used for transportation, and personal effects or burial plans that meet program rules. Documenting assets requires clear statements, statements of account, and proof of ownership to satisfy MDHHS reviewers and to avoid application delays. Exemptions reduce apparent resource totals and can be instrumental when spend-down is being calculated, because exempt assets do not need to be spent or altered to meet eligibility. Families should review program-specific guidance and prepare records that show how each asset is categorized to streamline eligibility determination and to understand whether spend-down will be required.
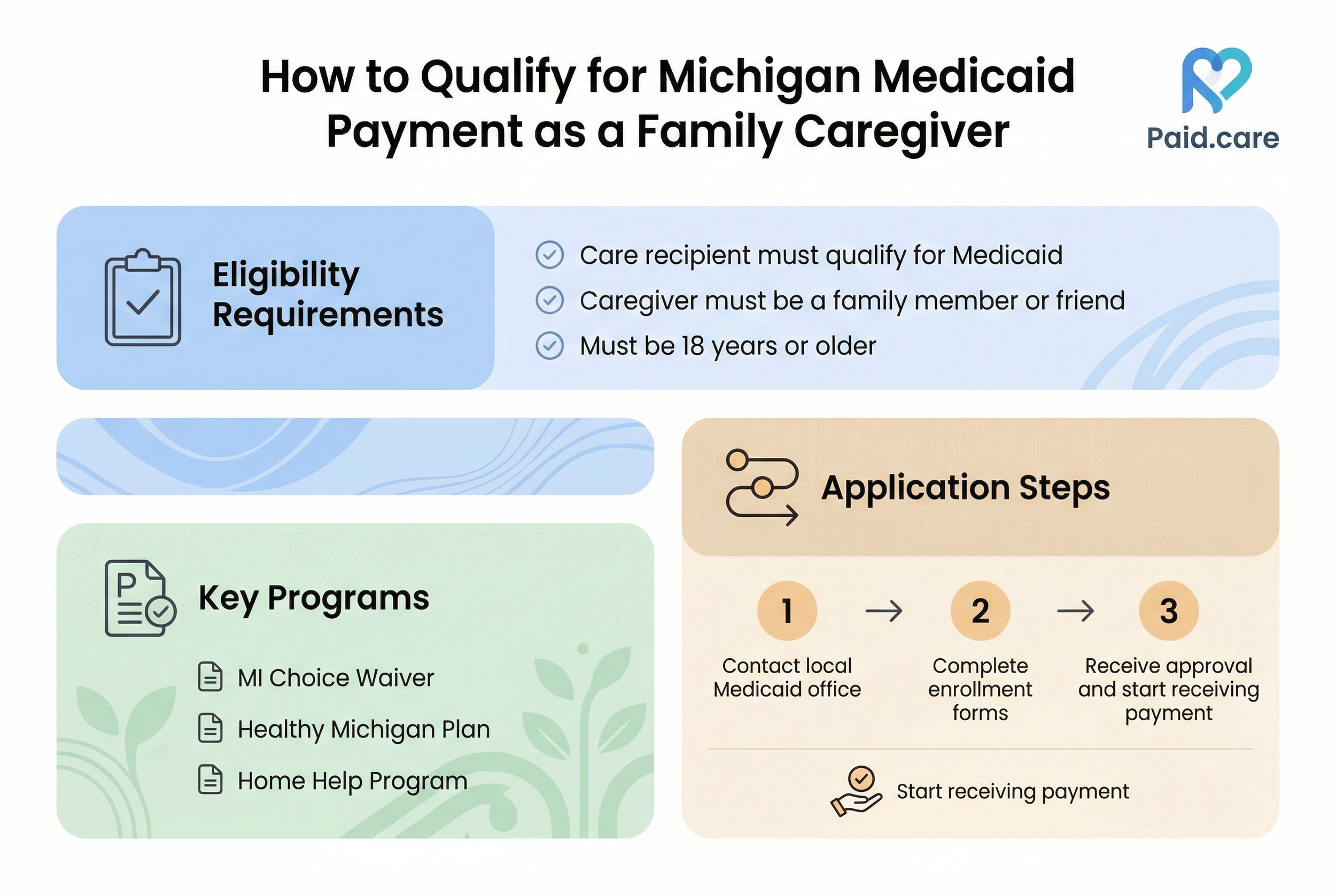
How Can Family Caregivers Qualify for Medicaid Payment in Michigan?
Family caregivers qualify for payment primarily when the care recipient meets program eligibility for services that permit consumer direction, and when program rules allow relatives to be employed as paid caregivers under employer-of-record arrangements. Eligibility scenarios typically center on the care recipient’s income and asset eligibility, documented functional need, and whether the service model supports consumer direction; spouses, adult children, and other relatives can often be paid if the program’s employer-of-record and conflict-of-interest rules are satisfied. Preparing for application includes securing medical documentation of need, collecting income and asset evidence, and understanding background check or caregiver qualification requirements that some programs impose. The checklist below outlines steps caregivers should take to position themselves for payment under Michigan Medicaid, followed by a focused Home Help eligibility subsection.
Paid.care can assist caregivers in confirming eligibility and walking families through next steps to prepare documentation and enrollment paperwork.
What Are the Eligibility Criteria for the Michigan Home Help Program?
The Michigan Home Help Program covers individuals who require assistance with daily living due to a physical or cognitive impairment and who meet functional eligibility following an assessment; approval of Home Help can enable the consumer-directed hiring of family caregivers. Recipient eligibility typically requires documentation of need from a medical provider and a formal assessment that determines the number of authorized hours and types of tasks covered, such as personal care and household assistance. Caregivers who will be paid must meet employer-of-record rules, background check requirements, and any training or registration the program mandates; these administrative steps vary by county and program contractor. Enrolling requires an application, assessment, designation of a consumer-directed plan, and completion of payroll or employer paperwork so the caregiver can be paid legally and on schedule.
Prepare medical documentation and an authorization of need for Home Help assessment.
Complete any required caregiver background checks and employer paperwork.
Establish a consumer-directed plan that specifies tasks, hours, and pay arrangements.
Home Help therefore hinges on the recipient’s documented need and completion of the assessment process that authorizes consumer-directed services and caregiver compensation.
What Is the Step-by-Step Process to Apply for Michigan Medicaid?
Applying for Michigan Medicaid follows a clear sequence: complete the initial application (via MI Bridges or MDHHS channels), gather required documents, undergo functional and medical assessments if applying for in-home services, receive eligibility determination, and enroll in the approved program that permits caregiver payment. Timely applications hinge on correct documentation — proof of income, proof of identity, medical records, and asset statements — and on scheduling assessments promptly once the application is accepted. Below is a numbered, featured-snippet-friendly step list that breaks the process into actionable steps caregivers can follow to move from inquiry to payment authorization.
Paid.care is available as a practical assistive service for completing the application, scheduling assessments, and facilitating payments when families prefer hands-on help.
Gather documents: proof of income, ID, medical records, and asset statements.
Apply: submit the Medicaid application through the state portal or MDHHS intake.
Schedule assessments: arrange functional assessments for in-home services or waivers.
Receive determination: MDHHS issues eligibility and authorized service hours.
Set up consumer direction: complete employer-of-record and caregiver enrollment paperwork.
Begin payment: caregiver starts receiving pay after payroll and authorization are active.
How Does Paid.care Assist Caregivers with Medicaid Eligibility and Payment?
Paid.care assists family caregivers by providing eligibility checks, dedicated care coaching, and facilitation of weekly payments to caregivers enrolled through state Medicaid programs, HCBS, and consumer-directed programs. Their service model includes free care coaching to help caregivers understand program rules and required documents, 24/7 support to reduce administrative friction, and a dedicated mobile application that helps manage care schedules and communication between consumers, caregivers, and program administrators. Paid.care’s role is to streamline the steps that commonly cause delay — confirming which program fits the recipient, organizing documentation for MI Bridges or MDHHS, and helping set up payroll so caregivers receive weekly payments. Caregivers ready to verify eligibility can use Paid.care’s check eligibility option to begin an assessment of whether their situation aligns with Michigan Medicaid payment pathways.
This concise description positions Paid.care as a supportive facilitator while keeping the focus on program rules and application mechanics.
What Are Common Questions About Michigan Medicaid Income Limits and Caregiver Payment?
Caregivers frequently ask targeted questions about single-person income limits, asset caps, spend-down calculations, and whether spouses or adult children can be paid; concise answers help with quick decision-making and next steps. The final H3 provides a single-person income figure framed in annual and monthly terms and clarifies which programs that figure applies to, optimized for rapid reference. Following the direct answer, additional short Q&A items address common PAA-style concerns that guide families to the relevant sections above for fuller explanations. These answers are designed to serve as quick checks before completing an application or contacting a care coach.
What Is the Income Limit for Medicaid in Michigan for a Single Person?
For many MAGI-based adult programs in 2025, the commonly cited threshold is 138% of the Federal Poverty Level for a single person, which converts roughly to about $20,120 annually or $1,677 per month; specific program rules and non-MAGI pathways may differ. This single-person figure is a practical benchmark for initial eligibility screening but does not apply uniformly across non-MAGI programs such as certain aged, blind, and disabled categories that use different income standards or count income differently. Check the income thresholds in the income limits table earlier in this article to see how that single-person benchmark compares with program-specific thresholds and to determine whether spend-down or asset tests will also apply.
The single-person 138% FPL benchmark is therefore a starting point; program selection and assessment results ultimately determine caregiver payment eligibility.
FAQs
-
The Limit: For 2025, the gross monthly income limit for an individual applicant is $2,901. This is known as the "300% Rule" (300% of the SSI Federal Benefit Rate).
The Hard Cap: Michigan is strict regarding this waiver limit. Unlike some states, you generally cannot "spend down" your income to qualify for the MI Choice Waiver if you earn over $2,901. If your income exceeds this amount, you may be ineligible for the waiver, though you might still qualify for other "Medically Needy" (Group 2) Medicaid services that offer fewer benefits.
-
The Change: Yes, there is a significant change. Effective February 1, 2025, Michigan has raised the asset limit for a single applicant to $9,660 (up from the historical $2,000 limit).
The Details: This means an individual can keep up to $9,660 in countable assets (cash, savings, investments) and still qualify. One vehicle and the primary home (if the applicant lives there or has intent to return) are exempt and do not count toward this limit.
-
The Rule: Generally, no. Under Michigan’s primary "Home Help" program, spouses and parents of minor children are considered "responsible relatives" and cannot be hired as paid caregivers.
The Exception: You can hire other family members, such as adult children, siblings, nieces, nephews, or friends. If you need a spouse to be paid, you would typically need to look into non-Medicaid funding sources like long-term care insurance or specific Veteran Directed Care programs, as state Medicaid rules prohibit it.
-
The Rates: As of 2025, the reimbursement rate for individual caregivers in the Home Help program is approximately $15.92 to $16.25 per hour.
The Process: In this program, the care recipient is the "employer." The state deposits the funds or handles the payroll (often through a Fiscal Intermediary), but the caregiver must log their hours using the state's Electronic Visit Verification (EVV) system to ensure payment.
-
The Alternative: They may qualify for the "Group 2" Spend-Down (Medically Needy) program.
How It Works: In this model, you are assigned a monthly "deductible" based on your excess income. You must incur medical bills equal to that deductible each month before Medicaid kicks in to pay for the remaining care. Note that this coverage is often less comprehensive than the MI Choice Waiver and requires strict monthly accounting of medical expenses.