Medicaid Estate Recovery and Family Caregiver Pay: What You Need to Know to Protect Assets and Get Paid
Medicaid estate recovery is a federal requirement administered by state Medicaid agencies that can affect the assets of people who received certain Medicaid long-term services and supports; understanding it helps families reduce unexpected liabilities while exploring opportunities for lawful caregiver pay. This article explains what estate recovery is, who and what it applies to, and the common exemptions and look-back rules that determine recoverable assets. It also lays out practical asset-protection tools such as Lady Bird deeds and irrevocable trusts, describes how family caregivers can be paid through consumer-directed and Home and Community-Based Services (HCBS) programs, and maps state-specific steps for Indiana, Michigan, and Illinois. Readers will find checklists, comparison tables, and step-by-step guidance to apply for caregiver pay, plus a concise explanation of where professional financial coaching and service facilitators fit into the process. Throughout, the focus is on actionable planning—protecting a care recipient’s estate while enabling eligible family members to receive compensation under Medicaid and related programs.
What Is Medicaid Estate Recovery and How Does It Affect Your Assets?
Medicaid estate recovery is the process by which state Medicaid programs seek repayment from the estate of a deceased beneficiary for certain Medicaid benefits paid on their behalf, primarily long-term care costs. The mechanism works because federal law requires states to attempt recovery for medical assistance provided to individuals age 55 or older, with states carrying out the claim against probate estates or other assets.
Recovery typically targets probate assets such as bank accounts subject to probate, proceeds of a decedent’s home if not otherwise exempt, and certain other estate assets that pass through probate; this can reduce inheritances or require estate planning to preserve family property. Knowing which assets can be recovered and how states apply exemptions is essential to planning ahead to minimize exposure.
What Are the Key Rules and Exemptions in Medicaid Estate Recovery?
Key federal and state rules set the baseline for who is subject to recovery and which assets are usually exempt from claims, creating a framework families must navigate when planning. Federal law requires recovery for long-term care costs for beneficiaries age 55+, but states determine implementation details, exemptions, and hardship waiver processes; common exemptions include surviving spouses, minor children, and permanently disabled children.
Hardship waivers are available in many states to prevent undue burden on heirs, though criteria vary and require formal application to the state Medicaid agency. Understanding state variation and documenting exemptions—such as proving a surviving spouse lives in the home—helps families preserve assets and prepare to contest or request waiver relief when appropriate.
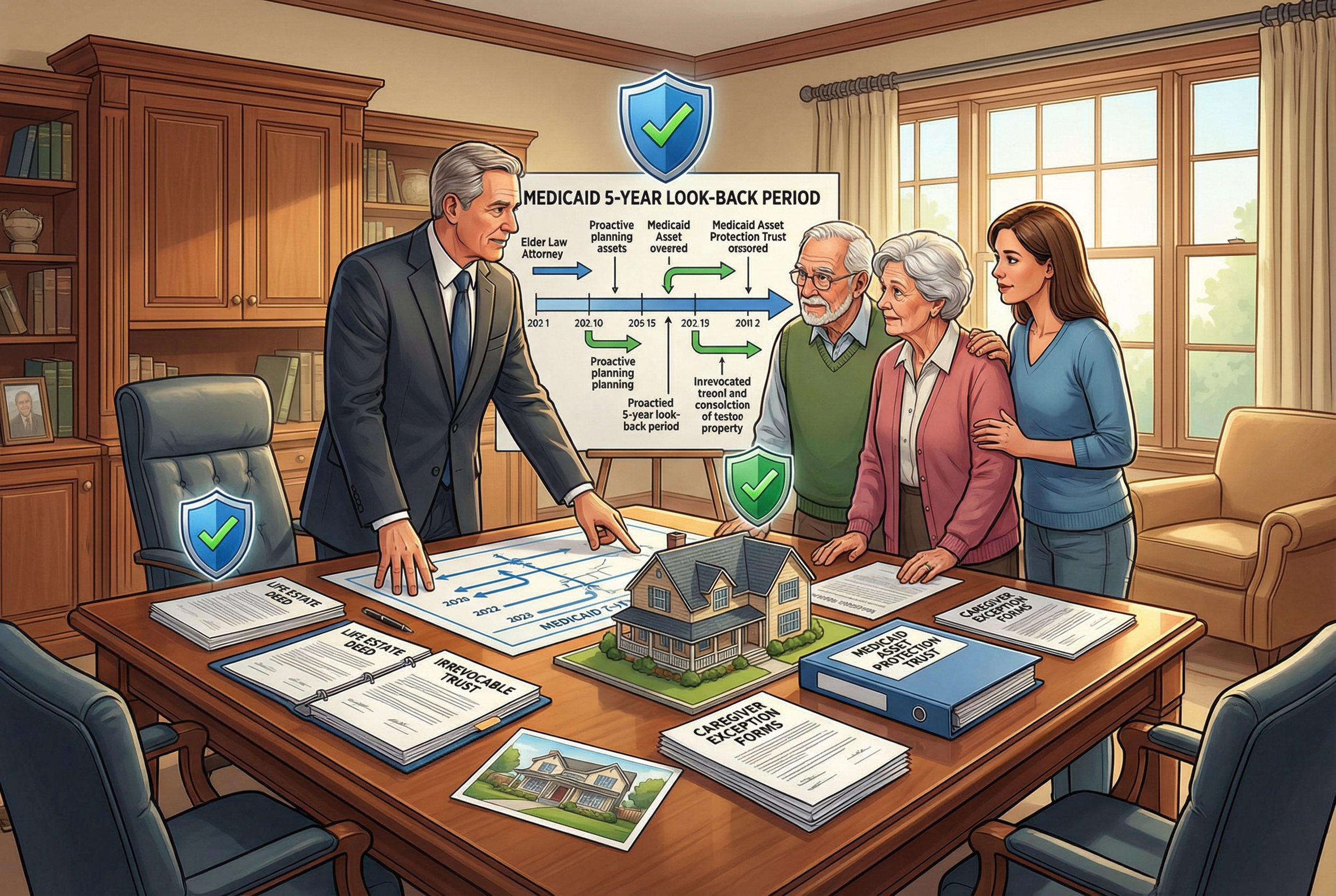
How Does the Medicaid Look-Back Period Impact Estate Recovery?
The Medicaid look-back period is a timeframe—commonly five years—during which asset transfers are examined to determine eligibility for Medicaid long-term care and to identify transfers that may trigger penalties. Transfers made within the look-back period that are not for fair market value can result in a period of ineligibility or be considered in recovery calculations, so timing and documentation of gifts or restructurings are critical.
Planning must therefore account for the look-back window: tools that protect assets often require setup well before Medicaid benefits begin to avoid triggering penalties. When transfers are necessary, clear records and legal advice reduce the risk of disqualification and subsequent recovery actions.
How Can You Avoid Medicaid Estate Recovery? Effective Asset Protection Strategies
Asset protection strategies aim to limit exposure to estate recovery while remaining compliant with Medicaid eligibility rules and the look-back period, using legal instruments and timing to manage risk. Common approaches include deeds and trusts that change how property is owned or titled, careful use of exemptions like the caregiver exception, and applying for hardship waivers when recovery would create undue hardship for heirs. Each tool has trade-offs: some require relinquishing control of assets or meeting strict timing rules, so choosing the right combination depends on the recipient’s care timeline and family goals. Consulting an elder-law attorney is crucial to ensure instruments like irrevocable trusts meet Medicaid asset protection trust requirements and are implemented before the look-back period would penalize transfers.
What Legal Tools Protect Your Home from Medicaid Estate Recovery?
Several legal instruments can protect a home from estate recovery when structured correctly and timed properly, each with distinct mechanisms and consequences. A Lady Bird deed (enhanced life estate deed) typically lets owners retain control while passing the home outside of probate, often preserving Medicaid eligibility while avoiding probate exposure; irrevocable trusts can remove assets from the applicant’s estate but usually require creation outside the look-back period to be effective. Life estates transfer remainder interests to beneficiaries but may create tax and control considerations, while Medicaid asset protection trusts are specialized irrevocable trusts intended to shield assets from recovery when established in compliance with state rules. Selecting the right tool depends on timing, the state’s rules, and the beneficiaries’ needs, so legal counsel is essential before making changes.
What Is the Caregiver Exception and How Does It Protect Your Estate?
The caregiver exception protects a home from estate recovery in specific circumstances by recognizing that a caregiver’s residence or services can justify an exemption, subject to state rules and documentation. Typically the exception applies when a spouse or dependent child resides in the home, or when a caregiver provides significant care that aligns with eligibility rules; states may exempt the home to avoid undue hardship on those living there.
To claim this exception, families generally must document living arrangements, caregiving responsibilities, and demonstrate how recovery would harm the caregiver or resident heirs. Proper documentation and early communication with the state Medicaid agency increase the chance the caregiver exception will be granted when eligible.
How to Get Paid to Care for Your Elderly or Disabled Family Member
Family caregivers can receive compensation through Medicaid-funded programs that allow consumer direction or designate family members as paid providers; these programs both provide income to caregivers and formalize care arrangements. The steps to become a paid caregiver generally include verifying the care recipient’s eligibility for HCBS or waiver services, completing provider enrollment and background checks, obtaining required training or certifications, and submitting time records for authorized services. Payment models vary—some programs use state payroll or employer-of-record arrangements while others reimburse family members directly—so understanding the program flow helps caregivers set up compliant payroll and documentation practices. A clear, step-by-step approach reduces delays in payment and ensures caregiving is recorded in a way that aligns with Medicaid rules.
Which Medicaid Caregiver Pay Programs Are Available in Indiana, Michigan, and Illinois?
State programs differ in name and structure, but Indiana, Michigan, and Illinois all offer HCBS waivers or consumer-directed programs that can pay family caregivers under qualifying circumstances; pay rates and program rules vary by state. Typical program elements include an eligibility determination based on functional needs, a care plan authorizing services that can be delivered by family caregivers, and a provider enrollment process that includes background checks and training. Below is a quick state reference tying programs to application steps and where a facilitator might assist.
After understanding state options, many families seek practical help to complete assessments and enroll caregivers efficiently; Paid.care acts as a facilitator to assist with eligibility checks, enrollment guidance, training, and administrative setup so families can move from approval to pay more quickly. Paid.care’s role includes eligibility screening, care coaching, and support for time tracking and payment workflows, and the organization notes features such as free care coaching, an app to simplify documentation, weekly payments, and around-the-clock support for qualification and setup—services that can be particularly helpful during the provider enrollment and payroll steps. Readers choosing assistance should confirm service fit and understand any enrollment requirements before relying on a facilitator.
What Are the Eligibility Requirements for Family Caregiver Pay?
Eligibility for family caregiver pay programs generally centers on the care recipient’s medical and functional needs and the caregiver meeting program provider standards, creating a dual-eligibility framework that both parties must satisfy. Common requirements include a documented need for assistance with activities of daily living, a formal care plan authorizing paid services, caregiver background checks and fingerprints in some states, and completion of any required training or competency checks. Employment status (W2 versus 1099) and payroll setup depend on program rules and employer-of-record arrangements, so tracking hours and maintaining payroll documentation is essential to avoid income counting or gifting pitfalls. Caregivers should compile identification, training certificates, and proof of relationship as part of the application packet to streamline enrollment.
Eligibility typically requires a formal assessment and a documented care plan authored by the state or care manager.
Caregivers usually must pass background checks and meet training requirements established by the program.
Employment and payroll procedures vary by state; caregivers should follow employer-of-record guidance to ensure compliant payments.
These core eligibility points clarify what families need to prepare before applying for caregiver pay; the next section outlines the broader landscape of programs that support caregiver compensation.
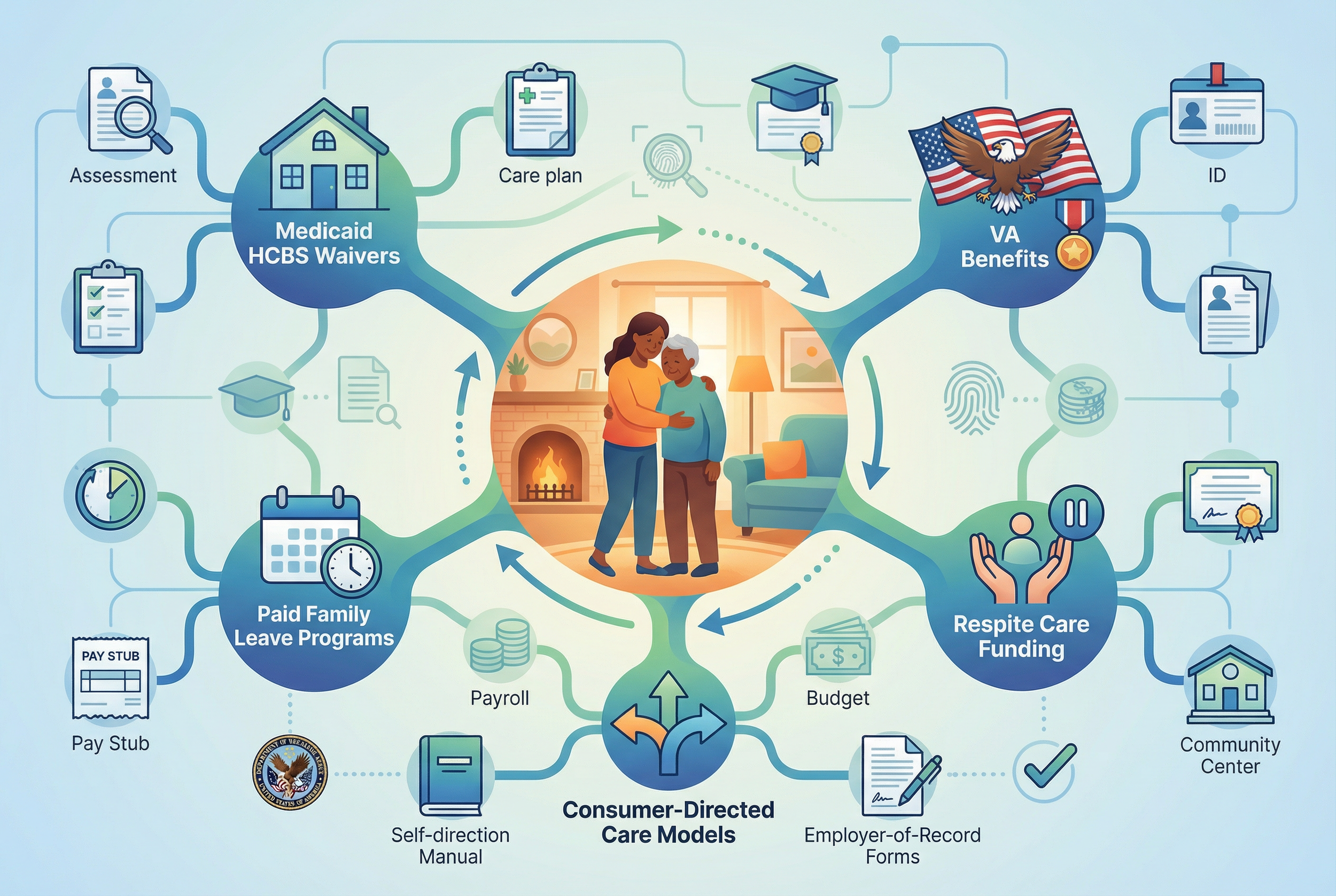
What Medicaid and Government Programs Support Family Caregiver Compensation?
A broader set of programs beyond Medicaid waivers can support family caregivers, including VA benefits for veterans, state paid family leave programs, respite care funding, and interactions with private long-term care insurance. Understanding how Home and Community-Based Services (HCBS) intersect with consumer-directed care models helps families see pathways to compensation and coordination across program types. Combining program options—such as leveraging VA aid and attendance benefits with state HCBS where permitted—can increase household resources available for caregiving while keeping compliance with Medicaid rules in mind. Knowing the program landscape helps caregivers assemble a benefits strategy that maximizes income while minimizing estate recovery risk.
How Do Home and Community-Based Services and Consumer-Directed Care Work?
HCBS programs provide long-term services in the community rather than institutional settings, and consumer-directed care allows an eligible recipient to choose and direct their caregivers, including some family members under specific rules. The process typically follows assessment → care plan authorization → provider enrollment → time tracking and payment, and self-direction often uses budgets or authorized service units that the recipient allocates to chosen providers. This model shifts certain employer-of-record responsibilities to the program or a fiscal intermediary, affecting payroll taxes and documentation for caregiver pay. Understanding whether a program is agency-directed or consumer-directed clarifies who handles hiring, supervision, and payment processing for family caregivers.
What Other Benefits Exist: VA Programs, Paid Family Leave, and Respite Care?
Several complementary benefits can augment caregiver income or provide temporary relief, and these intersect with Medicaid planning in practical ways families should consider. VA programs, such as aid and attendance or veteran-directed care, offer support for qualified veterans and their caregivers; state paid family leave laws may provide temporary wage replacement for some caregivers; and respite care programs provide short-term relief often funded through Medicaid waivers or nonprofit grants. Each source has distinct eligibility criteria and application processes, so combining benefits requires coordination and documentation to avoid affecting Medicaid eligibility or estate exposure. Exploring all available benefits provides a fuller picture of financial support for caregiving and can reduce reliance on estate assets.
How to Get Paid to Care for Your Elderly or Disabled Family Member
Family caregivers can receive compensation through Medicaid-funded programs that allow consumer direction or designate family members as paid providers; these programs both provide income to caregivers and formalize care arrangements. The steps to become a paid caregiver generally include verifying the care recipient’s eligibility for HCBS or waiver services, completing provider enrollment and background checks, obtaining required training or certifications, and submitting time records for authorized services. Payment models vary—some programs use state payroll or employer-of-record arrangements while others reimburse family members directly—so understanding the program flow helps caregivers set up compliant payroll and documentation practices. A clear, step-by-step approach reduces delays in payment and ensures caregiving is recorded in a way that aligns with Medicaid rules.
Which Medicaid Caregiver Pay Programs Are Available in Indiana, Michigan, and Illinois?
State programs differ in name and structure, but Indiana, Michigan, and Illinois all offer HCBS waivers or consumer-directed programs that can pay family caregivers under qualifying circumstances; pay rates and program rules vary by state. Typical program elements include an eligibility determination based on functional needs, a care plan authorizing services that can be delivered by family caregivers, and a provider enrollment process that includes background checks and training. Below is a quick state reference tying programs to application steps and where a facilitator might assist.
After understanding state options, many families seek practical help to complete assessments and enroll caregivers efficiently; Paid.care acts as a facilitator to assist with eligibility checks, enrollment guidance, training, and administrative setup so families can move from approval to pay more quickly. Paid.care’s role includes eligibility screening, care coaching, and support for time tracking and payment workflows, and the organization notes features such as free care coaching, an app to simplify documentation, weekly payments, and around-the-clock support for qualification and setup—services that can be particularly helpful during the provider enrollment and payroll steps. Readers choosing assistance should confirm service fit and understand any enrollment requirements before relying on a facilitator.
What Are the Eligibility Requirements for Family Caregiver Pay?
Eligibility for family caregiver pay programs generally centers on the care recipient’s medical and functional needs and the caregiver meeting program provider standards, creating a dual-eligibility framework that both parties must satisfy. Common requirements include a documented need for assistance with activities of daily living, a formal care plan authorizing paid services, caregiver background checks and fingerprints in some states, and completion of any required training or competency checks. Employment status (W2 versus 1099) and payroll setup depend on program rules and employer-of-record arrangements, so tracking hours and maintaining payroll documentation is essential to avoid income counting or gifting pitfalls. Caregivers should compile identification, training certificates, and proof of relationship as part of the application packet to streamline enrollment.
Eligibility typically requires a formal assessment and a documented care plan authored by the state or care manager.
Caregivers usually must pass background checks and meet training requirements established by the program.
Employment and payroll procedures vary by state; caregivers should follow employer-of-record guidance to ensure compliant payments.
These core eligibility points clarify what families need to prepare before applying for caregiver pay; the next section outlines the broader landscape of programs that support caregiver compensation.
What Medicaid and Government Programs Support Family Caregiver Compensation?
A broader set of programs beyond Medicaid waivers can support family caregivers, including VA benefits for veterans, state paid family leave programs, respite care funding, and interactions with private long-term care insurance. Understanding how Home and Community-Based Services (HCBS) intersect with consumer-directed care models helps families see pathways to compensation and coordination across program types. Combining program options—such as leveraging VA aid and attendance benefits with state HCBS where permitted—can increase household resources available for caregiving while keeping compliance with Medicaid rules in mind. Knowing the program landscape helps caregivers assemble a benefits strategy that maximizes income while minimizing estate recovery risk.
How Do Home and Community-Based Services and Consumer-Directed Care Work?
HCBS programs provide long-term services in the community rather than institutional settings, and consumer-directed care allows an eligible recipient to choose and direct their caregivers, including some family members under specific rules. The process typically follows assessment → care plan authorization → provider enrollment → time tracking and payment, and self-direction often uses budgets or authorized service units that the recipient allocates to chosen providers. This model shifts certain employer-of-record responsibilities to the program or a fiscal intermediary, affecting payroll taxes and documentation for caregiver pay. Understanding whether a program is agency-directed or consumer-directed clarifies who handles hiring, supervision, and payment processing for family caregivers.
What Other Benefits Exist: VA Programs, Paid Family Leave, and Respite Care?
Several complementary benefits can augment caregiver income or provide temporary relief, and these intersect with Medicaid planning in practical ways families should consider. VA programs, such as aid and attendance or veteran-directed care, offer support for qualified veterans and their caregivers; state paid family leave laws may provide temporary wage replacement for some caregivers; and respite care programs provide short-term relief often funded through Medicaid waivers or nonprofit grants. Each source has distinct eligibility criteria and application processes, so combining benefits requires coordination and documentation to avoid affecting Medicaid eligibility or estate exposure. Exploring all available benefits provides a fuller picture of financial support for caregiving and can reduce reliance on estate assets.
FAQs
-
Medicaid estate recovery is a process where the state may seek repayment for certain Medicaid benefits from a person’s estate after they die. In many states, this includes long-term services and supports (LTSS) like home care, nursing home care, and sometimes self-directed or consumer-directed caregiver programs. When a family caregiver is paid through Medicaid, those payments are usually considered part of the elder’s Medicaid-covered care. That means the total cost of care Medicaid paid for (including caregiver services) may be added up and potentially subject to estate recovery later, depending on state rules.
-
Not directly—but it can indirectly affect the amount Medicaid tries to recover. Medicaid estate recovery is based on what the program spent, not on whether the caregiver was a family member or an agency worker. If a self-directed program pays you, Medicaid still records those as care expenses. The more services Medicaid pays for, the larger the potential recovery claim. Whether the house is affected depends on how the home is titled, whether there’s a surviving spouse or disabled child, and your state’s specific rules. Some states limit or defer recovery when there are certain surviving relatives or when recovery would cause undue hardship.
-
Sometimes, yes—but it requires planning. Families may be able to:
Use a proper written caregiver agreement that clearly outlines duties and pay
Explore exemptions and hardship waivers related to the home and estate recovery
Look at options like life estates, transfer-on-death deeds, or special needs planning, when appropriate and allowed
Coordinate caregiver pay with Medicaid planning so that payments are fair-market, documented, and not seen as gifts
Because rules differ widely by state, it’s wise to speak with an elder law or Medicaid planning attorney before making big decisions about the home or transferring assets.
-
A caregiver agreement (sometimes called a personal services contract) helps show that payments to a family caregiver are legitimate wages for real services, not hidden gifts. A good agreement typically:
Describes what care is provided (ADLs, transportation, meal prep, supervision, etc.)
States the hourly rate and schedule, consistent with local market rates
Explains how and when the caregiver will be paid
Is signed and dated by both the elder and caregiver before payments begin
This documentation can help Medicaid reviewers and estate recovery agencies see that money paid to the caregiver was compensation for work—not an attempt to move assets out of the elder’s name.
-
Because estate recovery and Medicaid rules are complex and state-specific, it’s smart to consult:
An elder law attorney or Medicaid planning attorney in your state
A Medicaid caseworker or eligibility specialist to understand program rules
A tax professional (CPA or enrolled agent) about how caregiver pay affects income taxes
In some cases, a financial planner familiar with long-term care and Medicaid
They can help you coordinate caregiver pay, Medicaid eligibility, and estate planning so you can support your loved one, get paid lawfully, and understand how estate recovery may impact the home and other assets.