Indiana Medicaid Income Limits 2025: Eligibility and Payment Guide for Family Caregivers
Indiana Medicaid income limits determine who can receive state-funded health coverage and whether a family caregiver can be paid through waiver programs, and this guide explains those thresholds and the practical steps families need to take. Readers will learn how income and asset rules are calculated, which waiver programs commonly allow caregiver payments, the enrollment and documentation process, and pragmatic strategies for managing income above limits. This article focuses on eligibility mechanics, the role of the Federal Poverty Level (FPL) in Indiana program rules, and actionable pathways for family caregivers seeking payment under Structured Family Caregiving, Attendant Care, and other HCBS waivers. By the end you will understand program differences, the asset rules that matter for long-term care eligibility, and clear next steps to pursue caregiver pay. Throughout the guide we integrate practical checklists, comparison tables, and examples of documentation and timelines so families can move from confusion to confident action.
What Are the Indiana Medicaid Income Limits for 2025?
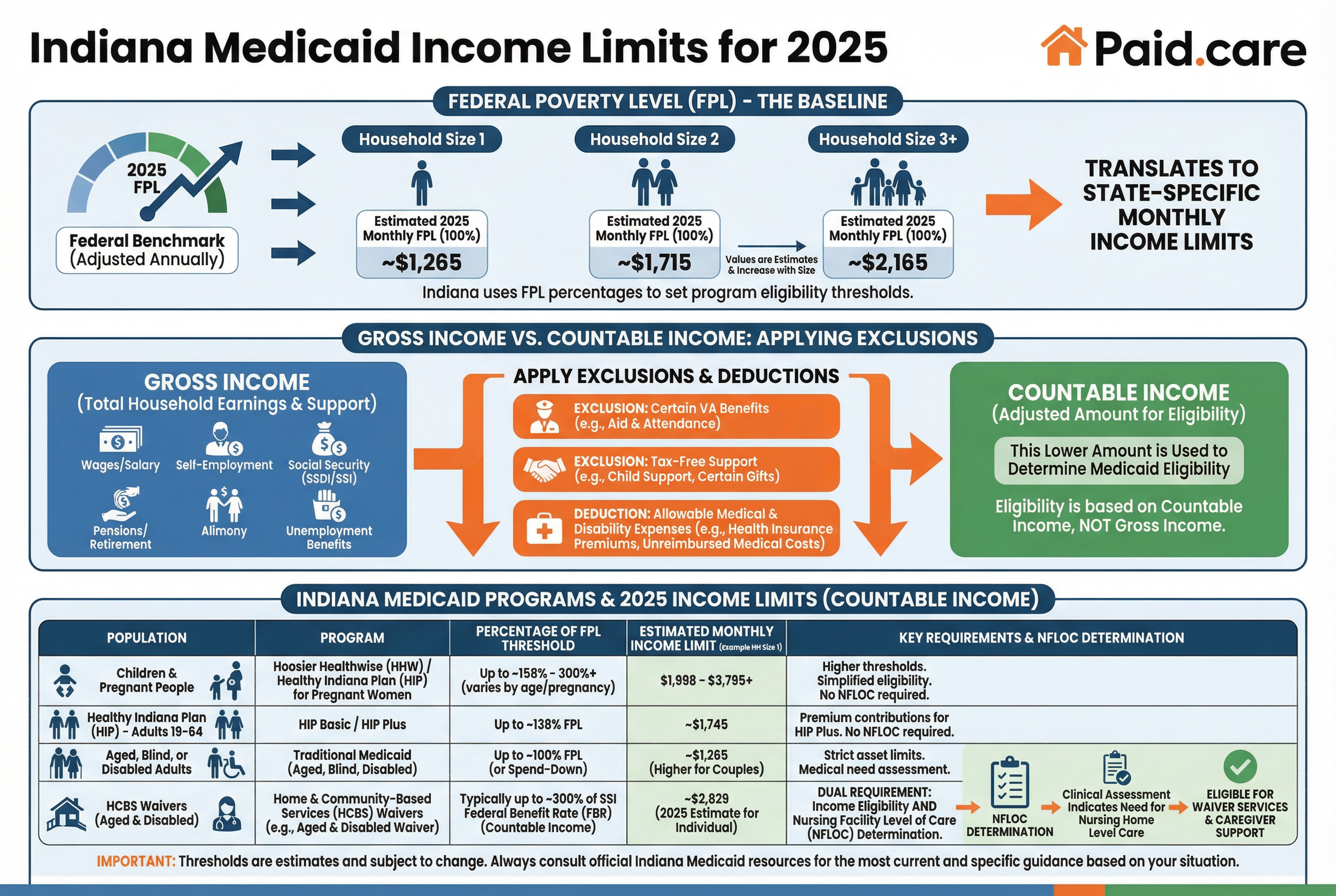
Income limits for Indiana Medicaid programs are program-specific thresholds that determine financial eligibility, typically expressed as a percentage of the Federal Poverty Level (FPL) or a state-set monthly amount. These limits exist because different programs serve distinct populations — children, adults, pregnant people, aged or disabled adults, and HCBS waiver recipients — so the applicable income test depends on the beneficiary category and the waiver rules. Understanding whether a person’s gross or countable income is used and how exclusions apply is essential to interpreting any headline limit.
How Are Income Limits Determined for Medicaid Eligibility?
Income limits begin with the Federal Poverty Level (FPL), a federal benchmark adjusted annually; Indiana maps program thresholds to the FPL or sets fixed monthly amounts derived from benefit standards. States typically translate a percent of FPL into monthly eligibility cutoffs and then apply rules to determine countable income, subtracting allowable exclusions like certain medical or disability-related expenses. The distinction between gross income (total received) and countable income (after deductions and exclusions) is crucial because a family may exceed gross thresholds but qualify after allowable exclusions are applied. Common income exclusions include some VA benefits, certain tax-free support, and program-specific medical deductions, and these exclusions directly affect whether someone qualifies for waivers that pay caregivers. Understanding FPL linkage and common exclusions helps families anticipate whether they must pursue spend-downs or trust strategies to qualify.
These income-determination mechanics lead directly into how program-specific limits vary across Indiana’s Medicaid landscape.
What Are the Income Limits for Different Medicaid Programs in Indiana?
Different Medicaid programs apply different income tests: some set thresholds based on a fixed percent of FPL, others use categorical eligibility rules, and some apply medically needy or spend-down calculations. For example, child and pregnant-person coverage often allows higher percent-of-FPL thresholds, while HCBS waivers for aged or disabled adults may require both Medicaid eligibility and a nursing-facility level-of-care (NFLOC) determination. Programs like Healthy Indiana Plan and Hoosier Healthwise typically use clear FPL-related brackets tied to household size, whereas waiver programs may rely on a combination of income tests and clinical eligibility. Families should compare program rules, because an adult who is income-eligible for one program may need a different approach—such as using allowable deductions or applying to a specific waiver—to enable caregiver payment eligibility. The comparison table above provides a starting point for which program style applies to a given situation.
How Do Indiana Medicaid Asset Limits Affect Eligibility?
Asset (resource) limits define what countable resources an applicant may hold while still qualifying for Medicaid; these limits are particularly important for long-term care and waiver eligibility because assets can disqualify otherwise income-eligible people. Countable assets generally include cash, savings, investments, and some non-exempt real property, while common exemptions typically cover the applicant’s primary residence (within equity limits), one vehicle, certain burial arrangements, and household goods. Spousal impoverishment rules further affect how a married couple’s assets are treated by protecting a community spouse’s resources through a Community Spouse Resource Allowance (CSRA). Because asset rules determine eligibility and possible spend-down needs, families must inventory resources carefully and document exemptions to avoid unexpected denials.
What Assets Count Toward Indiana Medicaid Limits?
Countable assets are typically liquid or readily convertible resources such as cash, bank deposits, stocks, and some retirement accounts; these are assessed against Medicaid resource limits when evaluating eligibility. Exempt assets usually include the applicant’s primary residence (subject to an equity cap), one vehicle used for transportation, household goods, personal belongings, and certain burial arrangements or prepaid funeral contracts. Edge cases—like annuities, jointly owned accounts, or recent transfers—can be treated as countable depending on structure and timing, and transfers for less than fair market value can trigger penalties or look-back periods. Families should compile clear documentation for each asset, prove the applicability of exemptions, and seek case-manager or legal counsel when complex asset arrangements exist. Accounting for these distinctions reduces the risk of denial and shortens the time to enrollment.
These asset definitions set the stage for how spousal impoverishment protections operate when one partner applies for long-term care Medicaid.
How Do Spousal Impoverishment Rules Impact Asset Limits?
Spousal impoverishment rules exist to prevent the community spouse from becoming destitute when the other spouse needs Medicaid-covered long-term care, and in practice they establish a Community Spouse Resource Allowance (CSRA) that permits the non-applicant spouse to retain a statutory minimum and maximum amount of resources. The CSRA formula and allowable amounts are set at federal guidance levels but administered by the state; the community spouse may retain resources up to the maximum allowance while the institutionalized spouse’s countable assets are assessed against Medicaid limits. These protections also influence income allocation and may allow the community spouse a larger share of joint resources, thereby impacting eligibility for caregiver payment programs that require the applicant to meet strict resource limits. Because rules can be complex and numbers change, couples facing this situation should document household resources accurately and consult elder-law counsel for planning to preserve family resources while pursuing Medicaid eligibility.
Knowing asset treatment and spousal protections helps families choose the right waiver pathway and avoid costly missteps when seeking paid caregiving arrangements.
Which Indiana Medicaid Waiver Programs Include Income Limits?
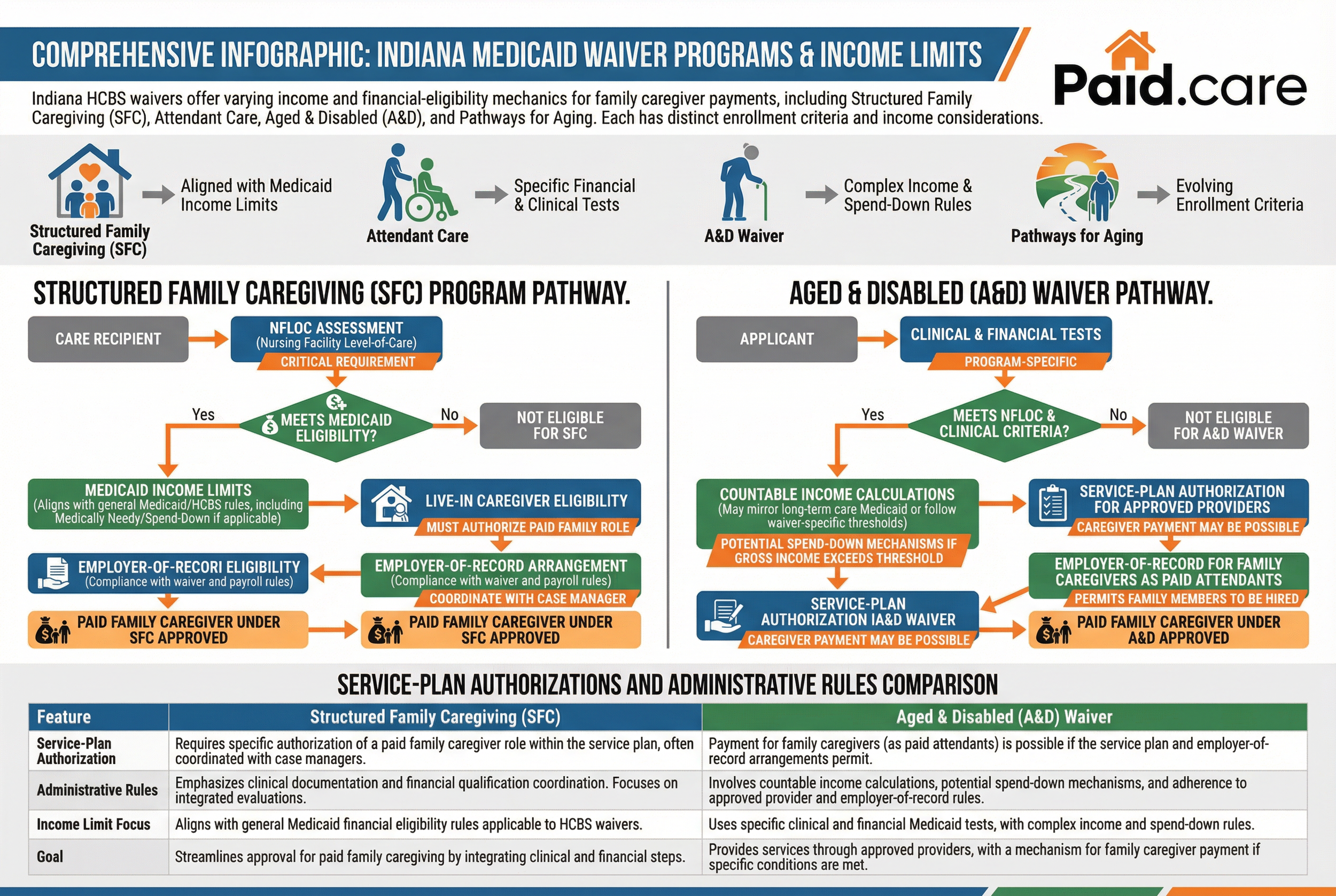
Indiana operates several Home and Community-Based Services (HCBS) waiver programs with varying income and financial-eligibility mechanics; some waivers explicitly allow family caregiver payments under structured programs while others have more restrictive rules. Key waivers relevant to family caregiver payment include the Structured Family Caregiving program, Attendant Care, Aged & Disabled (A&D) waiver, and PathWays for Aging, each with distinct enrollment criteria, NFLOC requirements, and income considerations. Some waivers apply the state Medicaid income rules directly, others require a separate financial assessment, and some programs may offer caregiver payments only when specific worker qualifications and employer-of-record arrangements are met.
Families should review waiver descriptions and negotiate service plans with case managers to confirm whether caregiver payment is allowable under the chosen waiver. The next subsections look more closely at Structured Family Caregiving and Aged & Disabled program rules.
What Are the Income Limits for the Structured Family Caregiving Program?
The Structured Family Caregiving (SFC) program is designed to permit payment to family members who provide care when the care recipient meets Medicaid eligibility and a nursing-facility level-of-care assessment. Income limits for SFC align with Medicaid financial eligibility rules applicable to HCBS waivers, meaning applicants generally must meet Medicaid income tests or qualify through medically needy/spend-down pathways where applicable. Live-in caregiver eligibility and NFLOC findings are critical: the care recipient must meet clinical need thresholds and the service plan must authorize a paid family caregiver role. Because SFC integrates clinical and financial evaluations, families should work with case managers to document the recipient’s care needs, confirm financial eligibility, and ensure that caregiver employment arrangements comply with waiver and payroll rules. Careful coordination of clinical documentation and financial qualification streamlines approval for paid family caregiving under SFC.
These program-specific income mechanics contrast with the Aged & Disabled waiver and its enrollment approach.
How Do Income Limits Apply to the Aged and Disabled Waiver?
The Aged & Disabled (A&D) waiver requires applicants to meet both clinical and financial Medicaid eligibility tests; income rules may mirror those used for long-term care Medicaid or follow waiver-specific thresholds depending on program design. Unlike some targeted family-caregiver waivers, A&D typically focuses on providing services through approved providers, but caregiver payment may be possible if the service plan and employer-of-record arrangements permit family members to be hired as paid attendants. Income treatment under A&D can involve countable income calculations and potential spend-down mechanisms if gross income exceeds the threshold; families must also ensure the recipient meets NFLOC or other clinical criteria to qualify. Comparing A&D to SFC and Attendant Care highlights the importance of service-plan authorizations and administrative rules in determining whether family caregivers can be paid under each waiver.
Understanding waiver-specific income application clarifies the practical steps families must take to get caregivers paid.
How Can Family Caregivers Get Paid Through Indiana Medicaid?
Family caregivers can be paid through Indiana Medicaid by following pathways that combine clinical eligibility (NFLOC), financial eligibility (Medicaid income and asset rules), and administrative enrollment in a waiver that permits caregiver payment. Common payment pathways include Structured Family Caregiving, Attendant Care arrangements, and select HCBS waivers that authorize paid family members when certain provider, training, and employer-of-record conditions are met. Key prerequisites are a formal assessment demonstrating NFLOC, documentation of Medicaid eligibility for the care recipient, selection and approval of a waiver or service plan that includes paid caregiver tasks, and completion of employment setup such as provider enrollment or home-care employer registration. Below is a concise numbered list of the practical steps families typically follow to secure caregiver payment.
Follow these essential steps to move from eligibility to payment for a family caregiver:
Determine Medicaid eligibility and confirm countable income/assets for the care recipient.
Obtain a nursing-facility level-of-care (NFLOC) assessment to document clinical need.
Identify and select the appropriate waiver or program that allows family caregiver payment.
Complete waiver application, service plan, and employer/provider enrollment paperwork.
Establish timesheet and payroll systems, ensure caregiver training/certifications, and submit timesheets for payment.
Paid.care assists family caregivers in Indiana, Michigan, and Illinois to navigate state Medicaid and other government programs to receive payment for caring for elderly or disabled loved ones. Primary product: facilitating payment for family caregivers through Indiana Medicaid waiver programs (including Structured Family Caregiving and Attendant Care). UVPs listed in the SERP report include: simplifying Medicaid/waiver application processes, dedicated care coaching and 24/7 support, weekly payments and competitive pay rates (examples cited in report), training/certifications, a Paid.care mobile app for hour tracking, free care coaching and no fees for caregivers.
What Is the Process to Qualify for Caregiver Payment Programs?
The process to qualify for caregiver payment programs follows a predictable sequence of assessment, documentation, application, and employment setup, and being prepared at each stage shortens approval times. 1) Determine Medicaid eligibility: collect income and asset documentation and confirm whether the recipient qualifies under Medicaid or a medically needy pathway. 2) Clinical assessment: obtain a nursing-facility level-of-care evaluation to show the recipient needs hands-on assistance. 3) Waiver enrollment: choose the appropriate HCBS waiver, submit applications, and work with a case manager to draft a service plan that includes paid family caregiving tasks. 4) Employment setup and payment: enroll the caregiver as an approved provider or employee, complete required background checks and trainings, establish payroll or fiscal employer arrangements, and set up timesheet submission processes for regular payments.
Paid.care can streamline each of these steps by performing eligibility checks, preparing documentation, assisting with waiver applications, helping set up timesheet submission, and supporting payroll setup; families are invited to Check Eligibility or contact Paid.care for personalized guidance and support. This service shortcut can reduce administrative bottlenecks and accelerate the start of weekly payments for qualified caregivers.
How Does Paid.care Simplify Medicaid Income Limit Navigation?
Paid.care offers practical support to families navigating complex Medicaid income and waiver rules by combining care coaching with administrative assistance and technology for hour tracking and payments. Their services include eligibility checks, help with Medicaid and waiver paperwork, assistance arranging required trainings and certifications, and tools to submit timesheets accurately through a mobile app—measures that reduce application errors and processing delays. Paid.care also emphasizes ongoing support: dedicated care coaching, 24/7 assistance, and weekly payment processing so caregivers receive predictable compensation once approved. For families seeking hands-on help with the Medicaid enrollment and caregiver-pay process, Paid.care provides a coordinated option to manage documentation, timesheets, and employer/provider setup without fees for caregivers; to begin, families can Check Eligibility or call for guidance.
These supportive services reduce administrative friction and allow families to focus on care while administrative partners manage program navigation and pay logistics.
What Are the Income Guidelines for Indiana Long Term Care Medicaid?
Income guidelines for long-term care Medicaid in Indiana differ from home- and community-based waiver rules because institutional care eligibility focuses on patient-pay calculations and maintenance needs in addition to basic Medicaid income tests. Nursing facility applicants must meet clinical NFLOC criteria and then undergo financial assessment where income above the limit typically becomes the patient’s share-of-cost, with the facility billing the patient or their representative for maintenance needs. HCBS waivers may treat income differently, sometimes allowing higher or alternative income thresholds when services are delivered in the community; therefore, families comparing institutional and community options should evaluate both clinical and financial consequences. The next subsections explain nursing-facility income treatment and practical strategies for managing income above Medicaid limits while preserving eligibility for needed services.
A clear comparison of institutional vs. waiver income approaches helps families choose the best care setting and financial strategy.
How Do Income Limits Differ for Nursing Facility Level of Care?
For nursing facility eligibility, income treatment centers on calculating a patient-pay or “share of cost” that accounts for the resident’s monthly income minus allowable personal needs allowance and other deductions, with the remaining amount applied toward facility charges and Medicaid covering the balance. This differs from many HCBS waivers that may allow services without the same patient-pay dynamics or may use different income thresholds linked to FPL. Institutional eligibility requires both clinical NFLOC confirmation and financial assessment; some income sources may be excluded from patient-pay calculations, while others count fully. Families should prepare for the facility billing process, understand allowable deductions, and collect documentation to minimize surprises in the monthly patient-pay calculation. Comparing these procedures with home-based waiver income rules informs whether pursuing a waiver to pay family caregivers is financially advantageous.
Understanding patient-pay mechanics leads into practical options for households with income or assets above standard limits.
What Strategies Exist for Managing Income Above Medicaid Limits?
When income exceeds Medicaid thresholds, families have several high-level, legally permissible strategies to consider: spend-downs that document excess medical expenses, Qualified Income Trusts (QITs or Miller Trusts) that redirect excess income into an irrevocable trust for care expenses, and careful timing of income recognition or benefit structuring to meet eligibility. Each strategy has rules and potential trade-offs: spend-downs require documented qualifying expenses; QITs have strict administration and are appropriate for those whose income alone would otherwise disqualify them; and legal or financial advisement is strongly recommended for complex cases. Families should avoid improper transfers of assets or unadvised maneuvers that could trigger penalties, and instead consult elder-law counsel or a knowledgeable case manager to determine the safest route. Implementing a compliant strategy can preserve access to Medicaid-funded care and, where applicable, enable the hiring and payment of family caregivers under approved waiver programs.
Careful planning and professional advice help families manage income issues while preserving eligibility for needed services and potential caregiver payments.
Paid.care assists families who prefer hands-on support through these financial and administrative steps by helping evaluate eligibility pathways and manage application paperwork; callers may Check Eligibility for personalized assistance. This supportive option can be especially helpful for households facing complex income or asset profiles that require careful documentation and timely filing.
FAQs
-
The Limit: For 2025, the gross monthly income limit for an individual applicant is $2,901. This figure is based on the "300% Rule" (300% of the Federal Benefit Rate, which is $967 for 2025).
The Detail: This limit applies only to the person needing care (the applicant). If the applicant is married, the income of their spouse is generally disregarded for eligibility purposes, provided the spouse is not also applying for Medicaid.
-
The Fix: Indiana is a "Miller Trust" state. If the applicant earns more than the limit (e.g., they have a high pension), they can still qualify by establishing a Qualified Income Trust (QIT), also known as a Miller Trust.
How It Works: Every month, the amount of income that exceeds the $2,901 limit must be deposited into this trust. The money in the trust is then used to pay the patient's "Patient Liability" (cost of care) or medical expenses, effectively lowering their countable income to zero for Medicaid purposes.
-
The Rates: As of mid-2025, the state pays provider agencies a daily stipend based on the level of care required. While the agency receives the full amount, they are required to pass through a percentage (typically roughly 60-70%) to you as the caregiver.
Level 1: Agency receives ~$77.54/day.
Level 2: Agency receives ~$99.71/day.
Level 3: Agency receives ~$133.44/day.
Your Take-Home: Expect your actual tax-free daily stipend to be lower than these gross figures (e.g., roughly $45–$85/day depending on the tier), as the agency retains a portion for case management and oversight fees.
-
The Rule: Yes. Unlike many other states, Indiana’s Structured Family Caregiving (SFC) program allows spouses to be the paid caregiver.
The Requirement: The spouse must live in the same home as the recipient and cannot have outside employment that conflicts with the care schedule. Note that under the older "Attendant Care" model, spouses were sometimes restricted, but SFC explicitly permits it.
-
The Limit: The applicant must have less than $2,000 in countable assets (cash, stocks, savings).
The Exemptions: The primary home is exempt (not counted) if the applicant lives there or intends to return, and the equity value is under approximately $713,000 (subject to specific 2025 adjustments). One vehicle is also exempt.
Warning: Indiana has a strict 5-year look-back period. If you transferred assets (like signing the deed of the house over to a child) within the last 5 years, Medicaid may impose a penalty period where they refuse to pay for care.