How to Adjust Caregiver Pay When Care Needs Increase: A Comprehensive Guide to Caregiver Pay Increase and Negotiation
Paid.care facilitates payment for family caregivers through government programs (state Medicaid programs, Home and Community Based Services (HCBS), consumer-directed programs, veteran-directed care programs, and paid family leave). This guide explains how to recognize measurable increases in care needs, how those changes translate into authorized hours or higher pay rates across public programs, and practical negotiation steps families and paid caregivers use to secure appropriate compensation. You will learn what kinds of clinical and behavioral triggers typically qualify for reassessment, how Medicaid waivers and VA budgets respond to escalating needs, and which documentation and market data best support a pay increase request. The article maps program mechanics (authorized hours, rate adjustments, budget authority), presents actionable steps to document increased tasks, and outlines immediate actions caregivers should take in light of current policy shifts. Throughout, we reference relevant program types such as Medicaid HCBS, Veteran-Directed Care, Paid Family Leave, and FLSA considerations so you can compare pathways and choose the most effective approach.
What Are Increased Care Needs and How Do They Affect Caregiver Pay?
Increased care needs are measurable changes in a person’s functional, medical, or behavioral status that require more caregiver time, higher-skill tasks, or constant supervision; these changes directly justify reassessment of authorized hours or approved pay rates. When needs escalate, programs adjust either the number of authorized care hours, an hourly rate or stipend, or reclassify the recipient into a higher level-of-care category that carries greater budget authority. For families and professional caregivers, recognizing the causal link between specific tasks and program mechanics is essential to making an evidence-based request for higher pay. The next subsections list the concrete qualifiers programs accept and show how escalation typically converts into compensation changes.
Which Care Needs Qualify for Pay Adjustments?
Care needs that commonly trigger pay adjustments include increased dependency in Activities of Daily Living (ADLs), onset or worsening of medical complexity, and cognitive or behavioral decline requiring supervision or specialized interventions. Examples include a person who now requires two-person transfers, needs tube feeding or complex wound care, or exhibits wandering and aggression that mandate continuous oversight. Programs often look for clinician documentation, incident reports, or rehabilitation notes showing a sustained change rather than temporary fluctuation. Gathering clear, task-focused evidence — such as frequency and duration of transfers or medication administration complexity — strengthens a request for increased authorized hours or a rate premium.
How Does Care Needs Escalation Impact Compensation?
Care needs escalation typically changes compensation through three mechanisms: an increase in authorized care hours, approval of a higher hourly rate or premium for specialized tasks, or allocation of additional budget authority (in consumer-directed or veteran programs). For example, adding two daily hours at a $20 hourly rate increases weekly pay by $280, while approval for complex-care premiums can raise the effective hourly compensation by 10–30%. Programs will usually require updated assessments, clinician notes, and a revised individualized care plan to reauthorize these changes. Preparing a simple calculation that multiplies new authorized hours by an appropriate hourly rate helps decision-makers see the practical budgetary impact of the request.
How Do Medicaid Programs Support Caregiver Pay Increases?
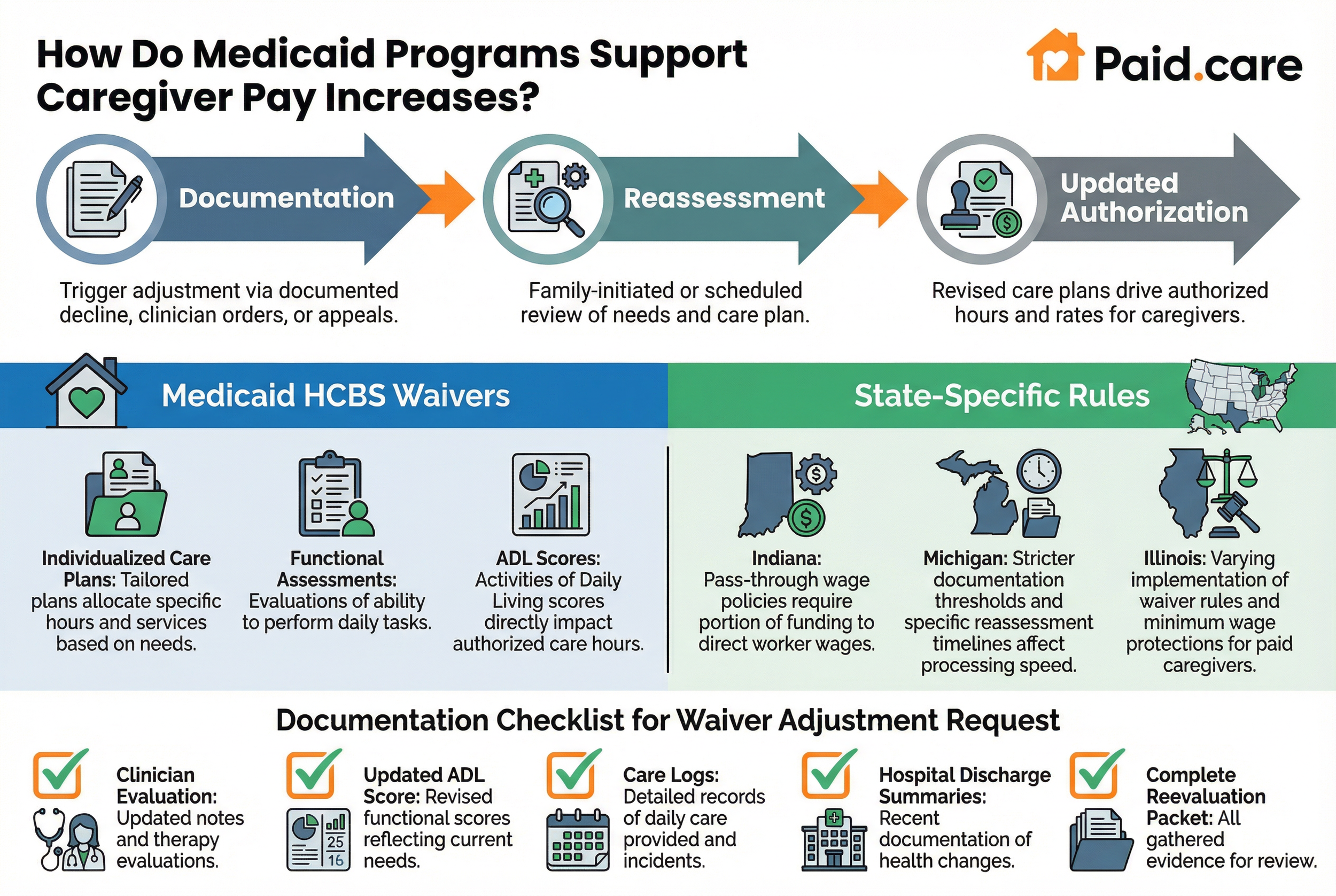
Medicaid supports caregiver pay increases through HCBS waivers, state plan options, and self-directed (consumer-directed) programs that allow individualized care plans to drive authorized hours and rates. Reassessment is typically triggered by documented functional decline, clinician-ordered changes, or family-initiated appeals that produce updated care plans. States differ in mechanisms and flexibility, but the core pathway is consistent: documentation → reassessment → updated authorization. Below is a comparison table that shows how common Medicaid pathways handle eligibility and adjustment mechanisms so families can compare triggers and likely outcomes.
What Are Medicaid Waivers and How Do They Adjust Pay?
Medicaid waivers, often called HCBS waivers, permit states to provide home and community-based services outside the standard institutional Medicaid rules and rely on individualized care plans to allocate hours and services. When a waiver participant’s needs increase, a reassessment or care-plan update drives authorization for additional hours or an increased rate for specialized care tasks. Evidence that strengthens a waiver adjustment request includes updated clinician notes, therapy evaluations, incident logs, and revised functional scores. A short checklist of documents — clinician evaluation, updated ADL score, care logs, and recent hospital discharge summaries — helps advocates prepare a complete reevaluation packet.
Which State-Specific Medicaid Rules Affect Pay Adjustments?
States vary widely in how they implement waiver rules, pass-through wage policies, and minimum wage or overtime protections for paid caregivers, and examples from states such as Indiana, Michigan, and Illinois illustrate these differences. In some states, pass-through rules require a portion of state funding to flow directly to worker wages, which raises baseline pay and can affect negotiation comparators. Other states set stricter documentation thresholds or differing reassessment timelines that change how quickly pay adjustments are processed. Families should check state-specific guidance and ask case managers about pass-through provisions and how often care plans are reviewed to anticipate the likely speed and size of any pay change.
What Veteran Benefits Increase Compensation for Family Caregivers?
The Department of Veterans Affairs offers several pathways that can increase caregiver compensation or the ability to pay family caregivers, most notably Aid and Attendance pensions, Veteran-Directed Care budgets, and caregiver support programs that allocate budget authority. These programs respond to increased dependency or clinical need by raising benefit amounts, expanding budget flexibility, or allowing veterans to use program funds to compensate family caregivers. Comparing key veteran programs clarifies which will respond directly to increased care needs versus which provide indirect budget flexibility for hiring or paying family caregivers.
How Does the Aid and Attendance Pension Benefit Adjust for Increased Care?
Aid and Attendance (A&A) is an income- and asset-based pension enhancement for eligible veterans or surviving spouses who need help with ADLs or require regular supervision; increased dependency can qualify an applicant for A&A or raise the assessed need level. An increased A&A award raises disposable income that families can use to pay caregivers or offset costs of hiring skilled help. Evidence to support an A&A adjustment includes physician statements describing ADL dependence, medication management needs, and documentation of falls or incidents. Filing or appealing an A&A decision typically requires consolidated medical evidence and a clear description of daily care tasks to justify a higher pension allotment.
What Is the Veteran-Directed Care Program and Its Pay Impact?
Veteran-Directed Care (VDC) provides a flexible budget that veterans and their caregivers can use to purchase goods and services that support community living, including paying family caregivers when allowable under program rules. When a veteran’s needs increase, the VDC team can re-evaluate the budget to allocate additional funds for caregiver compensation, assistive devices, or more hours of paid support. Budget increases are justified with updated clinical assessments and a revised participant plan of care that documents new tasks and hourly needs. Families using VDC should document additional task frequency and obtain provider corroboration to request a budget adjustment that permits increased payment to family caregivers.
How Can Family Caregivers Negotiate Higher Pay for Increased Responsibilities?
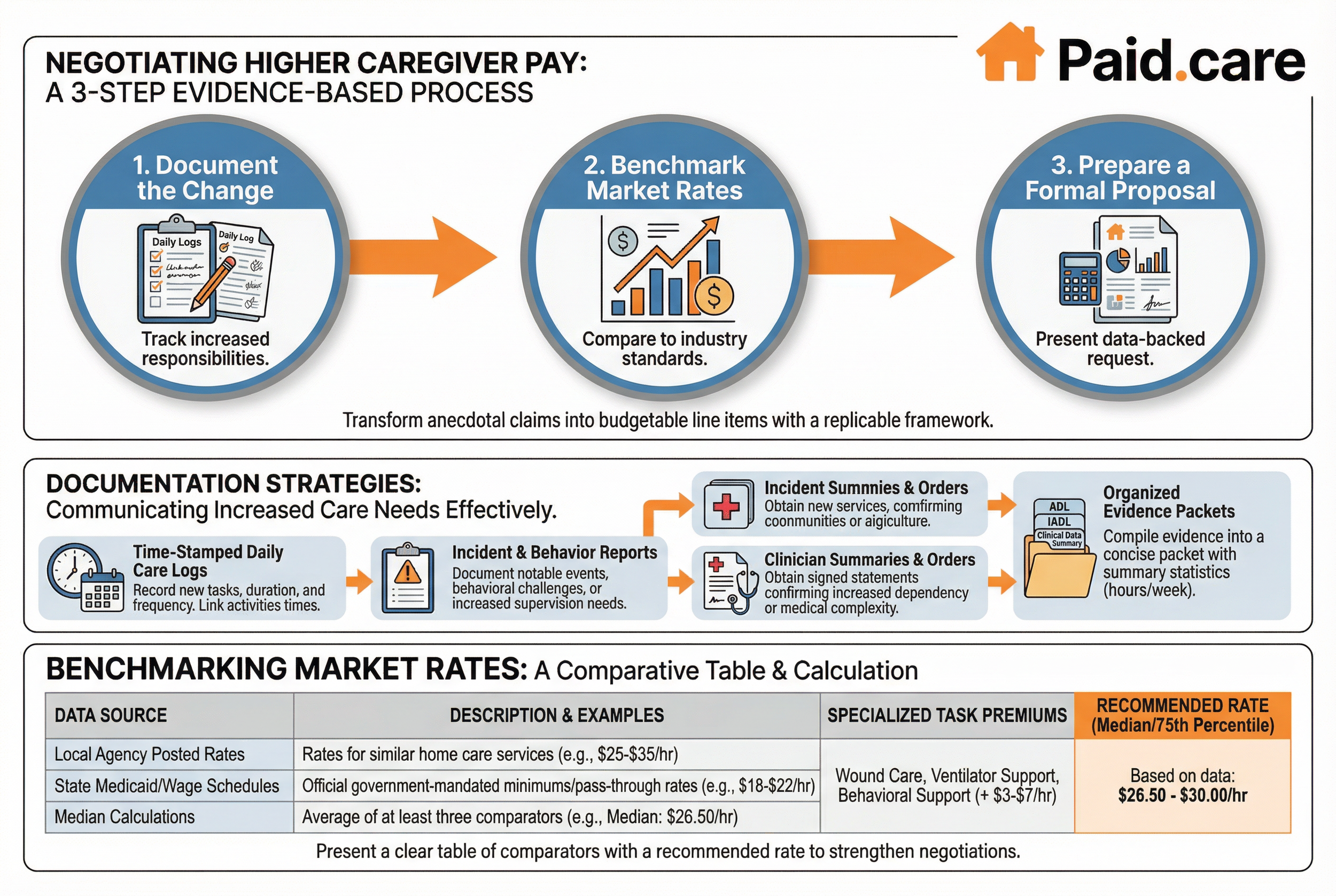
Negotiating higher pay begins with a structured, evidence-based approach: document the increased tasks, research market rates and program comparators, prepare a clear written request, and present a reasonable, data-backed proposal to the payer or household decision-maker. Effective negotiation treats the request as a budget-item change supported by quantifiable evidence, not simply a personal appeal. Below are practical steps that caregivers can follow to build a compelling case and convert increased needs into a formal pay adjustment.
Document the change: Keep daily logs, incident reports, and clinician notes that show new tasks and time required.
Benchmark market rates: Compare local agency rates, state pay schedules, and consumer-directed budgets to set a justified rate.
Prepare a formal proposal: Summarize evidence, show calculations (hours × rate), and offer a reasonable start date for changes.
These steps create a replicable framework that transforms anecdotal claims into budgetable line items, increasing the likelihood of a timely adjustment.
What Strategies Help Document and Communicate Increased Care Needs?
Strong documentation strategies include maintaining time-stamped daily care logs, incident or behavior reports for notable events, and obtaining signed clinician summaries that confirm increased dependency or medical complexity. Organize evidence into a concise packet: cover sheet with summary statistics (hours added per day/week), relevant clinical documentation, and a one-page narrative that ties tasks to ADL/IADL categories. Clinician signatures and objective measures (e.g., mobility scores) add credibility to a reassessment request. Presenting this organized packet to case managers, waiver coordinators, or family decision-makers makes it straightforward to convert documented need into authorized hours or rate adjustments.
How to Research Market Rates for Specialized Care?
Benchmarking market rates involves checking local home care agency posted rates, state Medicaid pass-through or wage schedules, and online job postings for specialized caregivers; combine these sources into a short comparison table that supports your requested rate. Use at least three comparators: two local agency rates and one state or regional pay schedule, then calculate the median to propose a defensible hourly rate. If available, include examples where specialized tasks (wound care, ventilator care, behavioral support) command a premium. Presenting a clear table of comparators with a recommended rate based on median or 75th-percentile figures strengthens negotiations and shows that the request aligns with market realities.
Which Other Government Programs and Paid Family Leave Support Caregiver Pay Increases?
Beyond Medicaid and VA pathways, paid family leave (PFL), state stipend programs, and long-term care insurance (LTCI) claims can provide temporary or supplemental income that supports caregivers during periods of increased need. These programs work differently — PFL provides wage replacement for eligible employees, state stipends may give small monthly payments, and LTCI can reimburse for paid caregiving or replacement services. Understanding when to deploy each option helps families create a layered support plan that protects caregiver income while pursuing program-based pay increases.
Paid Family Leave programs typically offer wage replacement for eligible workers who take time away to care for a seriously ill family member. PFL can temporarily replace income for an employed caregiver, making it a practical stopgap during acute increases in need. Below is a concise decision guide and set of examples that help determine when PFL is the right choice versus seeking programmatic pay increases.
PFL is best used when an employed caregiver needs time-limited leave to provide intensive care while maintaining job protection.
PFL benefits vary by state in duration and replacement rate, and using PFL can preserve household finances while applying for longer-term program changes.
PFL often interacts with short-term disability or employer leave policies, so coordinate claims to avoid coverage gaps.
How Does Paid Family Leave Benefit Family Caregivers?
Paid Family Leave (PFL) provides partial wage replacement and job-protected time for eligible employees who must care for a seriously ill family member, allowing them to maintain income during intensive caregiving periods. Benefit structures vary by state but commonly replace a percentage of wages for a defined duration, making PFL especially useful for acute episodes of increased need or during transitions while applying for program reassessments. PFL complements rather than replaces program-based pay increases because it is usually temporary and tied to employment status. When used strategically, PFL keeps household finances stable and buys time for longer-term funding pathways to be pursued.
What State Programs and Long-Term Care Insurance Options Are Available?
State-specific stipend programs and LTCI policies differ in eligibility, benefit size, and allowable uses, but both can help families offset caregiver income needs or pay for replacement care when family caregivers cannot meet heightened demands. LTCI claims often require documentation of need level and can reimburse for paid caregivers or agency services, while state stipends are typically smaller but easier to access. When pursuing these options, keep a concise claim packet with clinical documentation, care logs, and evidence of incurred caregiving expenses to support approval and maximize reimbursement. Combining LTCI reimbursement with state stipends and program adjustments offers a layered strategy for sustaining caregiver pay.
How Will Upcoming Policy Changes Affect Caregiver Pay in 2026 and Beyond?
Projected policy changes entering 2026 and beyond — including greater emphasis on passthrough rules for Medicaid HCBS, potential VA budget adjustments for caregiver programs, and FLSA overtime rule clarifications for home care agencies — will influence baseline market rates and the feasibility of paying family caregivers. If states increase passthrough percentages or expand self-direction options, more dollars may flow directly to worker wages or consumer budgets, improving the prospects for higher caregiver pay. Understanding these timelines and preparing documentation now positions caregivers and families to take advantage of policy shifts as they are implemented.
What Medicaid and VA Policy Updates Will Impact Caregiver Compensation?
Medicaid updates that increase passthrough requirements or expand consumer-directed options will likely translate into higher baseline wages or greater budget flexibility for consumers to compensate family caregivers. Similarly, VA policy changes that expand Veteran-Directed Care budgets or adjust Aid & Attendance thresholds could increase funds available for family caregiver pay. Monitoring state implementation timelines and preparing reassessment packets in advance — clinician documentation, up-to-date care plans, and clear hour calculations — will help families capitalize on these policy changes when they take effect. Caregivers should coordinate with case managers and care teams to ensure re-evaluation requests are submitted as state rules evolve.
How Will FLSA Overtime Rules Influence Agency-Employed Caregiver Pay?
Changes to FLSA overtime and minimum-wage rules for third-party agencies affect market baselines by raising agency-employed caregiver wages and altering typical hourly comparators used during negotiations. When agency rates increase due to overtime compliance, that creates a stronger market argument for raising family caregiver pay to remain competitive or to justify a higher private-pay rate. Families negotiating compensation can use updated agency pay scales as comparators in requests, showing that program-authorized rates or private arrangements should reflect current labor market conditions. Tracking local agency wage trends and FLSA implementation timelines gives caregivers concrete comparators to support pay increases.
Paid.care facilitates payment for family caregivers through government programs (state Medicaid programs, Home and Community Based Services (HCBS), consumer-directed programs, veteran-directed care programs, and paid family leave). Paid.care’s services include eligibility checks, documentation support, and pay facilitation via an app that helps track hours and manage payments. For caregivers seeking to quantify and present a compensation request, Paid.care’s pay calculator and care coaches can assist with eligibility screening, care-plan documentation, and preparing a clear packet for reassessment or negotiation. Paid.care also highlights program pathways in Indiana, Michigan, and Illinois where specific rules and pass-through policies influence the feasibility and size of pay increases.
Start with documentation: Compile clinician notes, daily logs, and a one-page summary of added hours and specialized tasks.
Use market comparators: Show local agency rates and state schedules to justify a proposed hourly rate or stipend.
Request reassessment formally: Submit the packet to the waiver case manager, VA team, or household decision-makers with a clear effective date for change.
This pragmatic sequence helps convert evidence of increased need into an actionable pay adjustment.
Paid.care facilitates payment for family caregivers through government programs (state Medicaid programs, Home and Community Based Services (HCBS), consumer-directed programs, veteran-directed care programs, and paid family leave). Contacting a care coach for an eligibility check, using a pay calculator to quantify a recommended rate, and preparing documentation with coach support are practical next steps for families and caregivers aiming to secure appropriate compensation in response to increased care needs.
FAQs
-
The Reality: No. Government programs (like Medicaid waivers or VA Aid & Attendance) and insurance providers are not automatically notified when a patient's condition worsens. They operate on the last assessment on file, which might be months or years old.
The Strategy: You must proactively request a "Change of Condition" Reassessment. Contact the case manager immediately and state clearly: " The care recipient has experienced a significant functional decline that requires increased service hours to ensure their safety."
-
The Rule: It depends on the funding source. In most state-run Medicaid programs (like IHSS in California), the hourly rate is fixed by the county or state and cannot be negotiated by an individual. In these cases, a "raise" effectively comes from being authorized for more hours per week.
The Exception: If you are paid through a "Consumer Directed" budget or private pay where the family controls the funds, you can negotiate a higher hourly wage if the complexity of care has risen (e.g., needing to learn wound care or tube feeding).
-
The Standard: Subjective statements like "It's harder now" will not work. You need to prove that the frequency or duration of specific tasks has increased.
The Strategy: Track "Paramedical" and ADL (Activities of Daily Living) changes. For example, if the recipient previously needed help to the bathroom 3 times a day but now is incontinent and needs changing 6 times a day plus skin care, document the exact extra minutes this adds to your daily routine.
-
The Context: Some home care agencies and long-term care insurance policies use "Tiered Pricing" (e.g., Companion Care vs. Complex Personal Care). If the recipient has moved from needing simple meal prep to needing physical transfer assistance (lifting), this pushes them into a higher tier.
The Fix: Ask your agency for their "Level of Care" descriptions. If your duties now match the description of a higher tier, write a formal letter requesting a re-classification of the client’s care plan, which typically triggers a higher billing and pay rate.
-
The Rule: Usually, the increase is effective from the date of the request or the date of the new assessment, not the date the health actually declined.
The Fix: This is why acting fast is crucial. Do not wait for the "annual review." Submit your request for a reassessment the moment the condition stabilizes at the new, lower baseline. Ask the case manager to confirm the "Effective Date" of the new authorization in writing.