How Paid Family Care Income Is Verified by Medicaid Programs: Eligibility, Verification, and Support
Paid family care through Medicaid means a state or federally funded long-term services and supports program authorizes payments to a family member who provides personal care to a Medicaid-eligible recipient. Verification matters because accurate income and hours checks determine whether payments are lawful, whether benefits continue, and whether audits can be defended. This guide explains the eligibility rules for both care recipients and caregivers, the paperwork and electronic systems agencies use to verify income and hours, program types that commonly pay family caregivers, state-specific practices in Indiana, Michigan, and Illinois, and financial planning tools that affect eligibility. For caregivers seeking practical help, Paid.care offers guided support—eligibility checks, free coaching, training, and mobile tools—to simplify document collection and tracking; readers can Check Eligibility with Paid.care to see program matches. The article is organized into clear sections: eligibility criteria, verification mechanics and tools, program types and verification differences, state-by-state highlights, financial planning strategies that influence Medicaid rules, and a focused overview of how Paid.care supports caregivers through verification and weekly payments.
What Are the Eligibility Criteria for Medicaid Paid Family Caregivers?
Eligibility for paid family caregiving under Medicaid depends on the care recipient meeting medical-need thresholds, the caregiver meeting program-specific relationship and training rules, and the recipient’s financial tests for Medicaid eligibility. States evaluate functional needs through ADL/IADL assessments and require caregivers to meet background checks, registration, or certification as defined by each program. Financial eligibility generally follows either MAGI-based rules for certain populations or SSI/non-MAGI rules for long-term services and supports, and assets/income are counted according to the program type. The practical result is that one household could qualify for a caregiver payment under a waiver but not under another program with a different asset test; that difference influences the verification steps caseworkers request. Understanding these three pillars—medical need, caregiver qualification, and financial tests—helps caregivers prioritize documentation and prepare for state assessments.
Eligibility for the care recipient is rooted in functional assessments that document need for assistance, which leads naturally into the specific assessment types used to evaluate ADLs and IADLs.
How Is Care Recipient Eligibility Determined Through Medical Needs and ADLs?
Care recipient eligibility is established through standardized assessments that document Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs), clinical notes, and provider or assessor statements. Assessors—often nurses, social workers, or interdisciplinary teams—score assistance needed for tasks such as bathing, dressing, toileting, mobility, medication management, and meal preparation, creating an evidence-based functional profile used to justify waiver or LTSS enrollment. Typical documentation includes a recent physician statement, a nursing assessment form, and observational notes detailing frequency and level of help; these items are combined to show the degree of dependence. For example, a person who needs two-person assist for transfers and daily help with medication management is likely to meet eligibility thresholds for many HCBS waivers. Clear, contemporaneous assessment records reduce rework during verification and make it easier for a family caregiver to be approved.
This assessment-driven approach leads into the companion financial eligibility tests that determine whether the care recipient qualifies under state income and asset rules.
What Are the Financial Eligibility Requirements Including Income and Asset Limits?
Financial eligibility depends on whether the program uses Modified Adjusted Gross Income (MAGI) rules or non-MAGI rules tied to SSI/Medicaid for long-term care, and whether assets are counted or protected through planning tools. MAGI-based programs focus on household income for certain groups, while non-MAGI long-term care programs apply stricter asset limits and may count income differently, often requiring spend-down or a Qualified Income Trust (QIT). States set asset thresholds and some programs exempt specific resources such as the primary residence or certain burial funds, though transfers during the look-back period can trigger penalties. Caregivers should obtain recent statements of countable income and assets for the care recipient, and consider consulting a qualified advisor before transferring assets. Gathering recent bank statements, retirement account summaries, and property documentation early helps streamline the verification workflow and avoid delays.
With financial rules clarified, the next section explains the exact mechanics that Medicaid agencies use to verify caregiver income and hours.
How Does Medicaid Verify Family Caregiver Income and Hours?
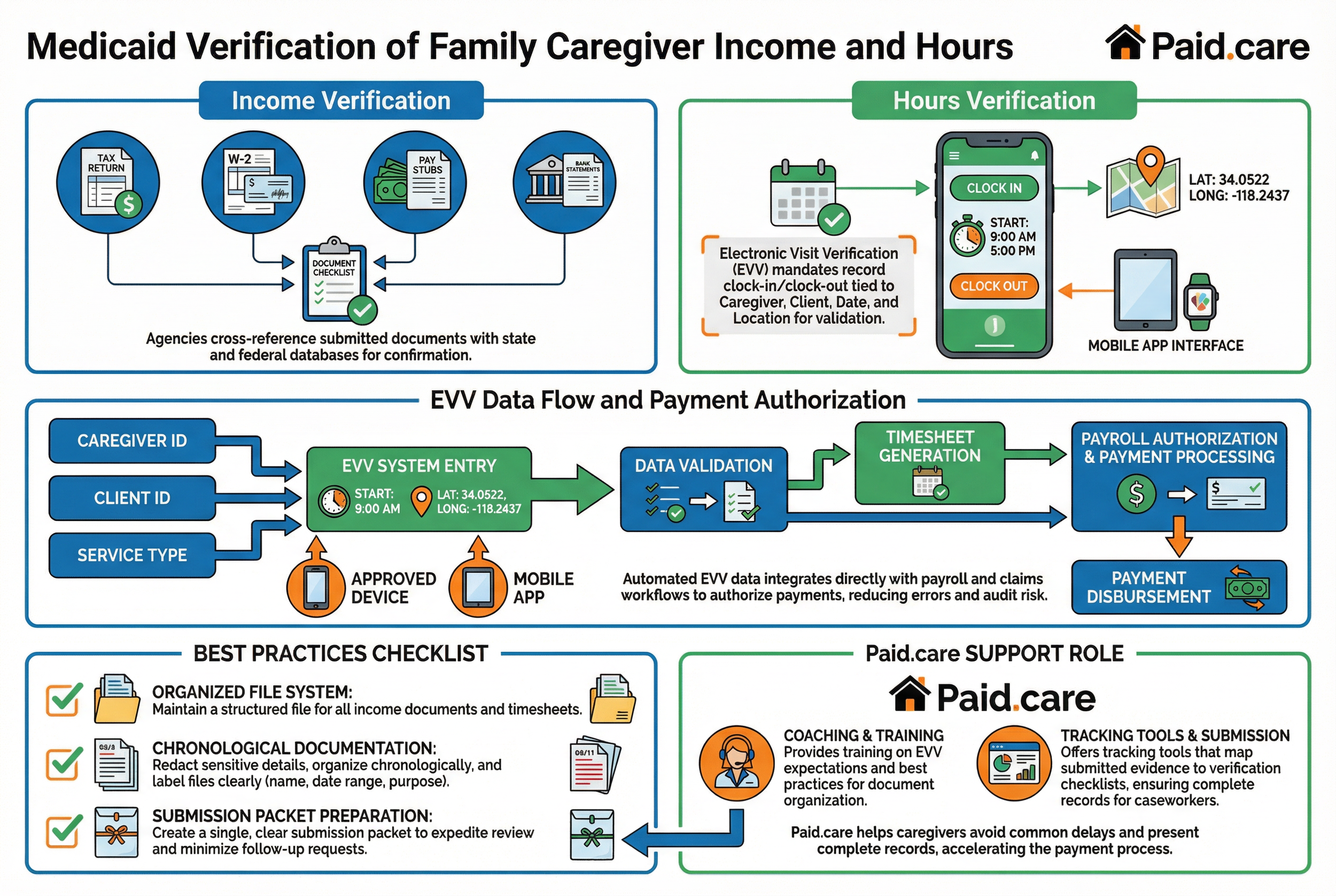
Medicaid verification of paid family caregiver income and hours combines document-based income checks, agency cross-referencing with state and federal databases, and time-tracking systems such as Electronic Visit Verification (EVV). Caseworkers request verifiable records—tax returns, pay stubs, W-2s, bank statements—to confirm income reported by caregivers or care recipients and to determine countable resources. Agencies reconcile submitted documents with program rules and may use state wage databases or other administrative matches to validate reported earnings. EVV systems, mandated for many personal care services under the 21st Century Cures Act, record clock-in/clock-out events tied to the caregiver, client, date, and location, and these electronic records are a primary source for hours verification and payment authorization. Because assembling documentation and learning EVV systems can be time-consuming, practical preparation—organized files and routine EVV practice—reduces audit risk and accelerates payment.
Paid.care assists caregivers here by coaching on document organization, training on EVV expectations, and offering tracking tools that map submitted evidence to verification checklists, which helps caregivers present complete records to caseworkers and avoid common delays.
What Documentation Is Required for Income Verification?
Income verification requires original or certified copies of income evidence that demonstrate earnings and resource levels for the care recipient and sometimes the caregiver, depending on program rules. Commonly requested items include the most recent federal tax return, W-2 forms, several months of pay stubs, and recent bank statements showing deposits. If tax returns are not available, alternative proof such as employer statements, unemployment paperwork, or notarized affidavits combined with bank documentation may be acceptable; agencies typically list acceptable alternatives in application instructions. Organize documents chronologically, redact unrelated sensitive details, and label each file with the name, date range, and purpose to make reviews faster. A clear checklist and a single submission packet cut down on follow-up requests and expedite verification.
How Is Electronic Visit Verification Used to Track Caregiver Hours?
Electronic Visit Verification (EVV) tracks caregiver hours by recording the who, what, when, and where of service delivery—typically caregiver ID, type of service, client ID, start/end times, and location data—through an approved device or mobile app. EVV data integrates with payroll and claims workflows so agencies can automatically authorize payments based on validated entries, reducing manual timesheet errors and audit risk. Common EVV problems include missed clock-ins, inaccurate location captures, and mismatched service codes; caregivers should be trained to confirm entries immediately after shifts to allow prompt correction. Privacy considerations require agencies to balance GPS or location stamping with client confidentiality; caregivers should follow state guidance on device use and data retention. Proper EVV practice ensures hours are traceable and payments are processed consistently.
Which Medicaid Programs Pay Family Caregivers and What Are Their Requirements?
Medicaid programs that commonly pay family caregivers fall into three broad types: Home and Community Based Services (HCBS) waivers, self-directed care programs (consumer-directed personal assistance), and Structured Family Caregiving (SFC) programs. Each model has different employer/payroll relationships, verification expectations, and eligibility nuances—waivers often involve case management and defined service caps, self-directed programs grant the care recipient or representative hiring authority with attendant verification needs, and SFC models may impose limits on services or cohabitation rules. Verification practices vary: waivers emphasize recipient functional assessments and financial tests, self-directed programs focus on caregiver enrollment, timesheets, and payroll processing, and SFC programs often have stricter documentation around relationships and allowable tasks.
What Are Home and Community Based Services Waivers and Their State Variations?
HCBS waivers are Medicaid authorities that allow states to provide home and community-based services to people who would otherwise need institutional care, with each state defining service mixes, provider rules, and eligibility thresholds. States often name waivers differently and set varying caps, enrollment priorities, and permissible paid caregiver roles, so verification steps can differ—some waivers require periodic reassessments, while others have fixed service authorizations. Key documentation typically includes a clinical assessment confirming the level of need, a care plan specifying approved services, and financial eligibility paperwork proving Medicaid enrollment. Because state implementation varies, caregivers should confirm the exact waiver name and forms required by their state Medicaid office to avoid failing verification on a technicality.
How Do Self-Directed Care and Structured Family Caregiving Programs Work?
Self-directed care programs give the care recipient or their representative budget or hiring authority to recruit and manage caregivers, often making the recipient the employer of record or delegating payroll to a fiscal intermediary, while Structured Family Caregiving programs limit who can be paid and the kinds of tasks that qualify for payment. In self-directed models, verification centers on caregiver enrollment, background checks, valid timesheets or EVV logs, and clear payroll authorization; in structured programs, agencies may require proof of familial relationship, cohabitation documentation, and strict task reporting. A simple scenario contrasts them: in self-directed care a family hires a neighbor and uses an EVV app to log hours for payroll, whereas in SFC a spouse may be eligible only under specified conditions and must meet additional program-defined checks. These operational distinctions determine the documentation caregivers must maintain to receive timely payment.
What Are the State-Specific Medicaid Paid Family Caregiver Programs?
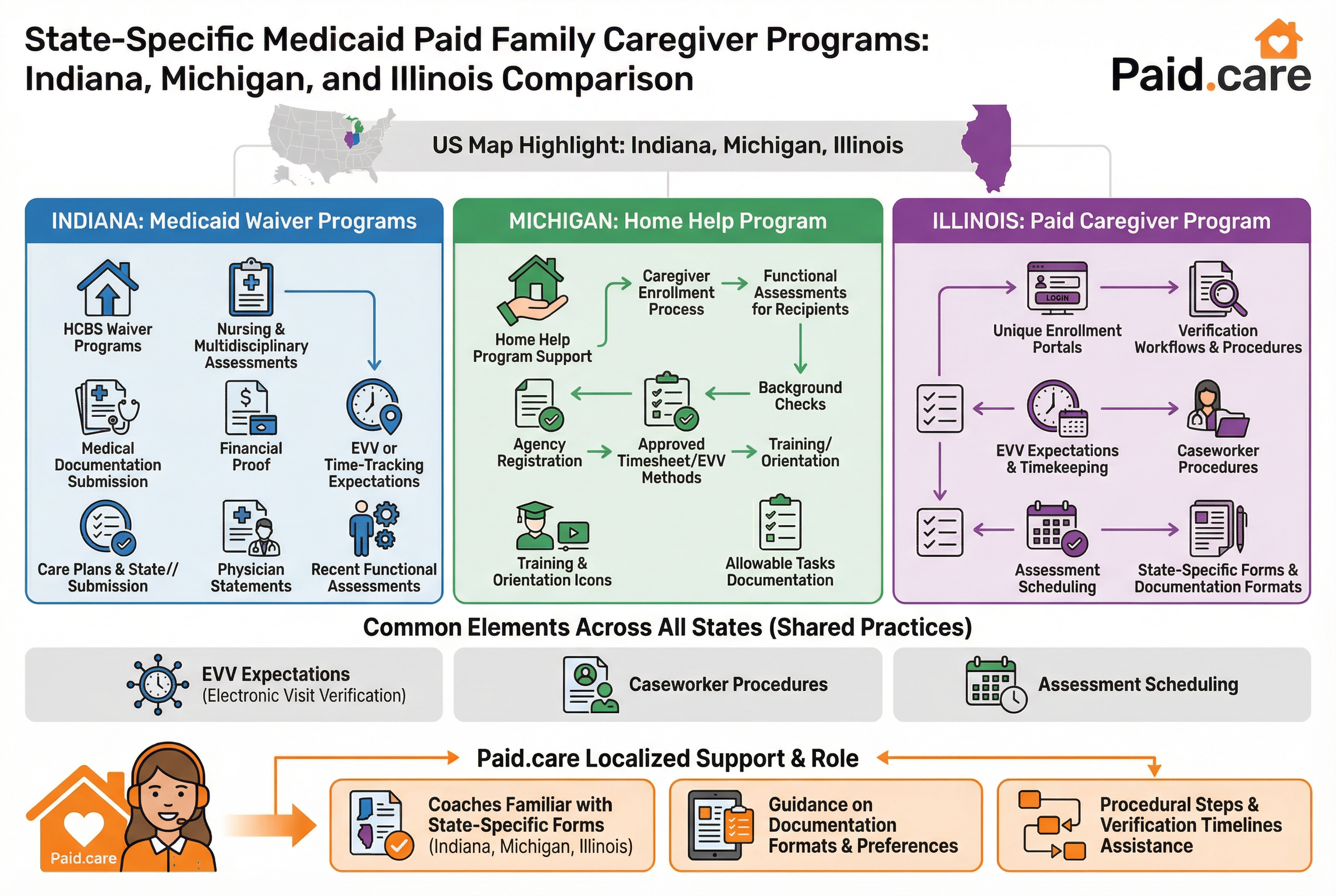
States implement paid family caregiver programs with differing names, forms, and verification workflows, so local rules determine the precise steps caregivers follow to qualify and get paid. Indiana, Michigan, and Illinois each operate HCBS waivers or home help-style programs with unique enrollment portals, EVV expectations, and caseworker procedures; understanding the local processes—how assessments are scheduled, which forms are required, and how EVV is implemented—shortens the verification timeline. Paid.care has experience in these states and offers coaches familiar with local practices who can point caregivers to the correct forms and procedural steps. Localized support is especially helpful for navigating state-specific subtleties such as documentation format preferences and the names of relevant waiver programs.
What Are the Key Features of Indiana’s Medicaid Waiver Programs?
Indiana’s waiver programs for home- and community-based services define eligibility through nursing or multidisciplinary assessments and require submission of medical documentation, care plans, and financial proof to the state or its designated agencies. EVV or time-tracking expectations apply for paid personal care, and caregivers commonly present physician statements and recent functional assessments during verification. Paid.care’s local coaches know the common Indiana forms and typical submission sequences, and they assist caregivers in gathering the assessments and income documents that Indiana caseworkers expect. Preparing a single, labeled packet with assessment forms, physician notes, current bank statements, and a clear caregiver enrollment form often eliminates iterative document requests and speeds authorization.
How Does Michigan’s Home Help Program Support Paid Family Caregivers?
Michigan’s Home Help program supports paid family caregiving through a structured caregiver enrollment process, functional assessments for recipients, and systems for recording hours that integrate with payroll and state reporting; caregivers must complete background checks, register with the appropriate agency, and use approved timesheet or EVV methods. Registration steps include submitting identity and eligibility documents, receiving training or orientation in some counties, and following state guidance on allowable tasks and recordkeeping. Paid.care’s coaches who work in Michigan can guide caregivers through registration, outline the documentation Michigan agencies typically request, and provide practical EVV training to minimize rejected claims or payment delays. Knowing the sequence—registration, assessment, documentation submission, and timesheet/EVV reconciliation—helps caregivers plan and maintain continuous compliance.
How Can Financial Planning Help Meet Medicaid Eligibility for Paid Family Caregivers?
Financial planning can affect countable income and assets for Medicaid eligibility through strategies such as Qualified Income Trusts (QITs), careful management of transfers during the look-back period, and leveraging exceptions like the child caregiver exception where applicable. Proper planning identifies which resources are countable under state rules and whether tools like QITs can stabilize monthly income calculations to meet eligibility thresholds. Advisors and caseworkers commonly recommend documenting the rationale for any transfers and ensuring property titles and account ownership reflect program requirements to avoid penalties. Effective planning reduces the chance that an otherwise eligible recipient will be denied due to preventable asset or income issues.
What Is a Qualified Income Trust and How Does It Affect Eligibility?
A Qualified Income Trust (QIT) is a legal vehicle that holds a Medicaid applicant’s income when state rules require countable income to fall below program thresholds; by directing certain income into the trust to pay allowable expenses, a QIT can make an otherwise over-income applicant eligible for long-term care benefits. Setting up a QIT involves drafting trust documents that comply with state Medicaid rules, naming an appropriate trustee, and following the state’s accounting and distribution requirements. Because QITs affect monthly income calculations and may have implications for reimbursement to the state after death, caregivers and applicants should consult qualified elder-law counsel before creating one. Properly administered, a QIT simplifies verification by providing clear, auditable records of how income is applied toward care costs.
How Do the Medicaid Look-Back Period and Child Caregiver Exception Impact Asset Protection?
The Medicaid look-back period requires states to review prior asset transfers for uncompensated gifts that could trigger penalty periods before eligibility, and penalties are calculated based on the value of transfers divided by the state’s payment rate for nursing-home care. Transfers within the look-back window can therefore delay eligibility, so documenting legitimate reasons and timing is critical. The child caregiver exception can exempt certain home transfers from penalty where a child provided care that allowed the owner to remain at home, but applicability varies by state and requires careful demonstration of facts. Practical steps include avoiding large uncompensated transfers during the look-back period, keeping detailed records of any transfers, and seeking legal advice to evaluate exceptions and protective strategies. Clear documentation simplifies verification and reduces the likelihood of a retrospective penalty claim.
How Does Paid.care Support Family Caregivers Through the Medicaid Verification Process?
Paid.care supports family caregivers by combining free coaching, step-by-step eligibility checks, and a mobile app that helps organize documents, train caregivers on EVV and timesheet practices, and track hours toward weekly payment. Coaches guide caregivers through assembling the precise evidence caseworkers request—assessments, physician statements, tax and bank documents—and provide training to reduce EVV errors and timesheet mismatches. The Paid.care mobile app facilitates eligibility checks, shift logging, care plans, in-app chat with care coaches, and weekly payment processing, helping caregivers move from initial application to first payment with fewer administrative hiccups. These services aim to reduce paperwork friction and speed verification without replacing professional legal or financial advice when complex planning tools are required.
Paid.care highlights include highest pay rate examples and practical supports which caregivers find useful when evaluating program fit.
Free care coaching: Coaches review documentation and explain next steps for verification.
Eligibility checks: The app offers guided checks to map caregivers to state programs.
Shift tracking and EVV support: Tools and training reduce common EVV and timesheet errors.
Weekly payment facilitation: Processes aim to accelerate routine caregiver payments.
What Free Care Coaching and Training Does Paid.care Provide?
Paid.care provides no-cost care coaching that helps caregivers identify required documents, prepare for assessments, and learn EVV or timesheet best practices, with coaches available to review packet completeness before submission. Typical coaching touchpoints include a checklist review of income and asset documents, step-by-step guidance on how to document ADLs/IADLs for caseworkers, and practical EVV onboarding showing how to clock shifts and correct common errors. Coaches also advise on preparing concise physician statements and organizing bank or tax records for quick review by caseworkers. Scheduling coaching sessions through Paid.care connects caregivers with local expertise tailored to Indiana, Michigan, and Illinois procedures when relevant.
How Does the Paid.care App Facilitate Eligibility Checks and Payment Tracking?
The Paid.care app centralizes eligibility check tools, secure chat with care coaches, care plan templates, and shift logging that aligns with EVV requirements and payroll processing to streamline verification and weekly payment cycles. Users can upload and label income and assessment documents, log shifts in a format consistent with state reporting, and communicate questions to coaches for rapid resolution of documentation issues. The typical timeline from sign-up to first payment involves an eligibility check, coach-supported document submission, EVV or timesheet setup, and validated hours being processed during the weekly payroll cycle. By keeping records organized and offering in-app support, the app reduces reconciliation errors and provides a clearer audit trail for agencies.
FAQs
-
The Mechanism: Medicaid programs now mandate Electronic Visit Verification (EVV). You must use a mobile app, landline, or dedicated device to "clock in" and "clock out."
The Check: The system captures your GPS location (or caller ID) at the exact moment you start and end your shift. If the GPS shows you are at the grocery store or your own home (if you don't live with the recipient) when you clock in, the payment will be flagged or denied.
-
The Mechanism: Yes. State agencies run automated "Data Match" audits. They compare the dates you billed for home care against the dates the care recipient was admitted to a hospital or skilled nursing facility.
The Risk: If you logged hours on a day the recipient was an inpatient (which is generally prohibited), the system will flag it as an "overpayment," and you will receive a demand letter to pay that money back.
-
The Challenge: Because many live-in caregivers qualify for the IRS Notice 2014-7 "Difficulty of Care" exclusion, this income may not appear on Line 1 (Wages) of your 1040 tax return, making it look like you have $0 income to lenders.
The Fix: You must provide "Alternative Documentation." Instead of just a tax return, submit your official pay stubs (which show the gross earnings) and a "Verification of Employment" (VOE) letter from your agency explaining that the income is stable but tax-exempt under federal law.
-
The verification: It depends on the benefit.
For MAGI Medicaid (ACA expansion): If the income is tax-exempt under IRS Notice 2014-7, it is generally excluded from your Modified Adjusted Gross Income (MAGI), meaning you may still qualify for free health insurance.
For SNAP: Most states do count this as earned income, as SNAP uses "Gross Income" rules that differ from IRS taxable income rules. You must report it, or you risk fraud penalties.
-
The Mechanism: Yes. Even if you don't file a tax return, the paying agency usually files a Form W-2 or 1099 with the IRS.
The nuance: If you are exempt under Notice 2014-7, the agency might report the wages in "Box 14" (Other) rather than "Box 1" (Taxable Wages), or you may receive a W-2 with $0 taxable wages but full Social Security wages. The IRS "sees" it, but acknowledges it is non-taxable for income tax purposes.