How Caregiver Pay Works During Temporary Care Gaps: Understanding Paid Family Caregiver Programs and Eligibility
Temporary care gaps are short periods when regular care is interrupted—such as during medical recovery, emergency leave, or planned respite—and they create immediate needs that government programs and consumer-directed models can help fill by paying family caregivers. This article explains how caregiver pay works during those short-term gaps, outlining the primary public programs that authorize payments, the typical eligibility rules, and the practical steps families use to get paid quickly. You will learn how Medicaid HCBS waivers, VA caregiver supports, state paid family leave, and respite voucher programs function as mechanisms to transfer funds or stipends to family caregivers, plus how consumer-directed programs let families hire relatives. The piece also covers application processes, documentation checklists, typical pay structures and rates, tax considerations, and strategies to maximize net benefits during temporary assignments. Finally, we describe practical tools and supports—including an app-based workflow and caregiver coaching—that reduce friction when arranging paid short-term care. Readers who want to act after learning the options will find clear, actionable steps for checking eligibility and starting the enrollment process.
What Government Programs Support Paid Family Caregivers During Temporary Care Gaps?
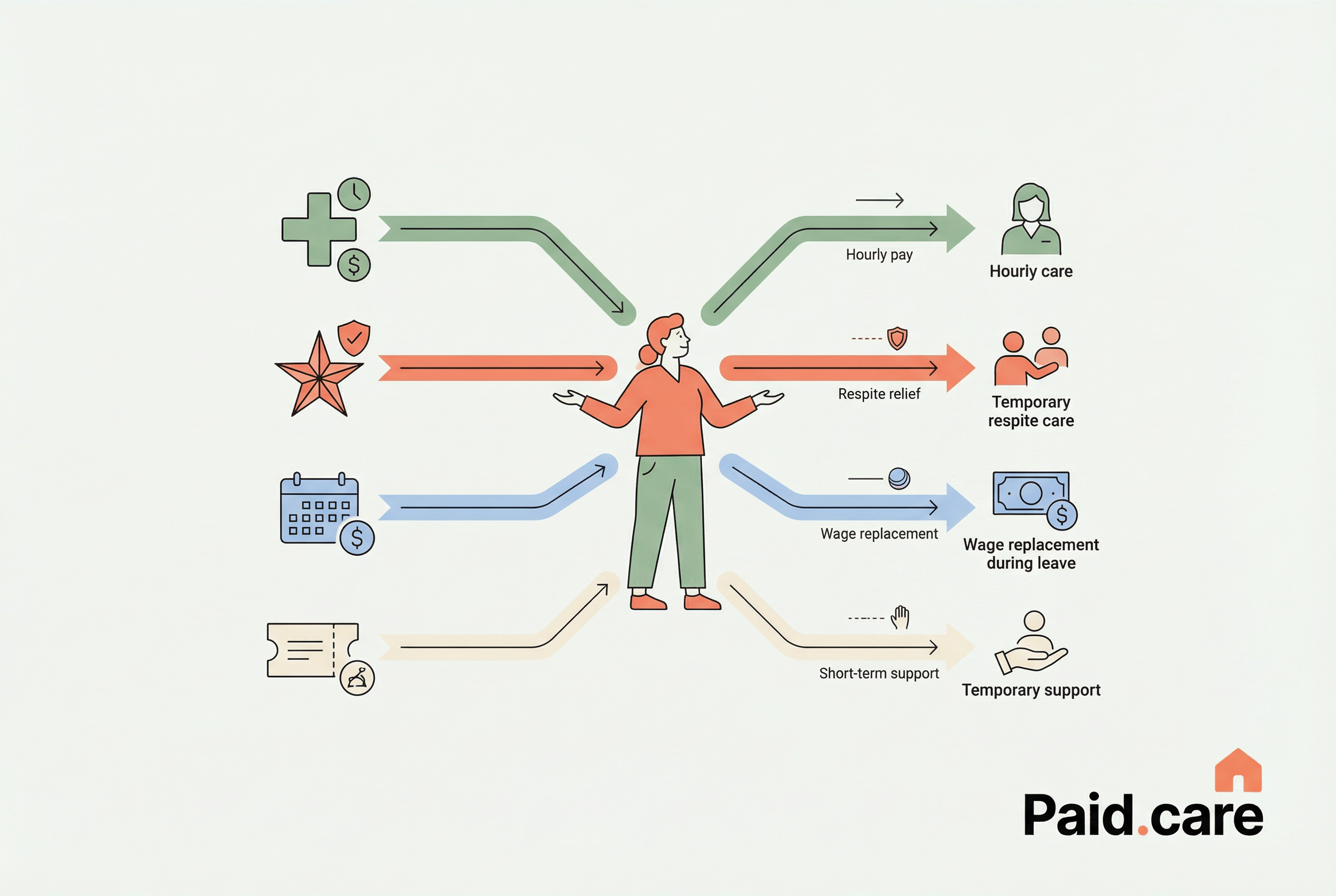
Paid family caregiving during temporary care gaps is supported primarily through four government avenues: Medicaid HCBS waivers and consumer-directed programs, VA caregiver and respite supports, state paid family leave wage-replacement programs, and targeted respite voucher programs for short-term relief. Each pathway operates under different rules—some pay hourly to a hired family caregiver, others offer stipends or wage replacement to the primary worker—so the mechanism determines who can be paid, for how long, and what documentation is required. Understanding these differences helps families match their immediate need (emergency leave, short surgery recovery, or planned respite) to the appropriate program quickly. Below is a compact comparison that highlights eligible situations and typical benefit types so caregivers can assess likely fits before applying.
How Does Medicaid Provide Caregiver Payment Eligibility for Respite Care?
Medicaid supports caregiver payment for temporary respite primarily through Home- and Community-Based Services (HCBS) waivers and consumer-directed personal assistance options that let the care recipient or their representative hire family members as paid providers. The mechanism works by including respite or short-term personal care in an approved care plan; once a care plan documents medical necessity and the state approves the waiver-funded service, a fiscal intermediary or employer agent can enroll and pay the family caregiver. The direct benefit is quick, authorized hours of paid care that replace or supplement usual services during a gap, but specifics—such as whether spouses are eligible or caps on hours—vary by state program rules. Caregivers should review the care plan criteria and request a respite authorization that clearly defines duration, scope, and pay rates.
Medicaid’s consumer-directed models rely on documented need and program enrollment, which naturally leads into how VA benefits compare as a source of temporary caregiver stipends and respite.
What VA Caregiver Stipends Are Available for Temporary Relief?
VA caregiver supports provide a mix of monthly assistance, caregiver training, and limited respite services that veterans and families can access when a veteran’s care needs create a temporary gap or require backup coverage. The mechanism typically combines a primary caregiver designation with approved services that include short-term respite days or contracted respite care, and occasionally stipend components depending on program enrollment and eligibility. For families, the main benefit is access to structured respite days and potential stipend support that reduces financial stress while the primary caregiver takes a brief leave. Accessing VA supports requires veteran eligibility validation and coordination with VA caregiver program administrators to schedule respite and confirm any short-term pay or stipend arrangements.
These VA supports form one practical route for temporary relief, and the next section explains the general eligibility criteria families must meet to be paid for short-term caregiving.
How Can Family Caregivers Qualify for Paid Care During Short-Term Care Periods?
Qualification for paid short-term caregiving hinges on three core elements: the care recipient’s clinical need and program enrollment, caregiver approval or enrollment under the program, and residency or program-specific administrative rules. Programs require a functional assessment that documents medical necessity and expected care tasks; that assessment drives hours, service types, and whether family members can be hired. Caregiver requirements often include proof of relationship, background checks in some programs, and formal enrollment or training completion—steps that determine whether a family member can be the paid provider. Understanding these three dimensions lets families target the fastest applicable route and prepare the required documentation for rapid approval.
Below are the eligibility checkpoints families commonly need to verify before applying for paid short-term care.
Medical and functional assessment confirming need for personal care or respite under program rules.
Care recipient’s active enrollment in Medicaid, VA program, or local respite voucher eligibility verification.
Caregiver identification, relationship proof, and any required background or competency checks.
What Are the Eligibility Criteria for Medicaid and State Programs?
Medicaid and state programs usually require a documented medical necessity—often via a functional assessment or care plan—that shows the care recipient needs assistance with activities of daily living or supervision. Financial eligibility or Medicaid enrollment is commonly required for many HCBS waivers, while some state respite or voucher programs focus only on need and residency rather than income. The care plan must specify services (respite hours, personal care tasks), and the caregiver often needs to enroll as a provider with supporting ID, relationship proof, and sometimes completed training or background checks. Preparing these items in advance shortens the approval window and ties directly into the application steps described later.
Which Family Relationships Qualify for Paid Caregiver Benefits?
Many consumer-directed programs allow a broad range of relatives—adult children, parents, siblings, and other kin—to be paid as family caregivers when the care plan authorizes it, but programs commonly place limits on spouses, legal guardians, or paid household members depending on state law. Some waivers explicitly permit payment to relatives except where state regulation or conflict-of-interest rules exclude particular relationships; others require an outside provider for certain tasks. These distinctions matter because who can be paid affects how quickly a family can source a caregiver during a temporary gap and whether additional approvals or waivers are needed. If relationship rules are unclear, contacting program administrators or using an eligibility check tool is the fastest way to confirm allowable paid providers.
Understanding eligibility and relationship rules leads to a practical, stepwise application process that helps families get paid quickly.
What Is the Application Process for Paid.care Services During Temporary Care Gaps?
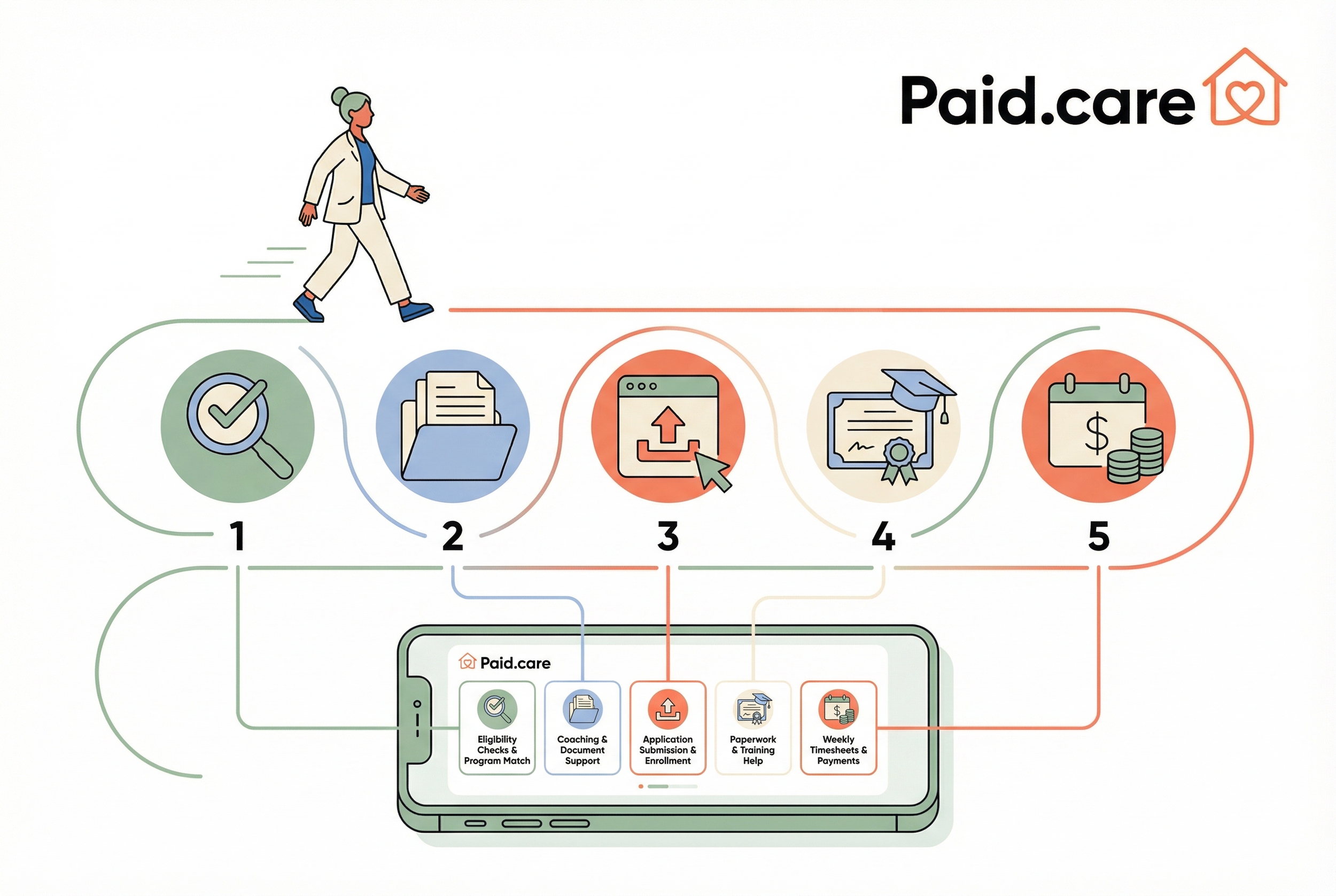
The application flow for enrolling in paid family caregiving combines eligibility screening, documentation preparation, program enrollment, and timesheet/payment setup; Paid.care assists caregivers through each step to speed approval and weekly payment delivery. The core mechanism begins with a program match: identifying which public program or combination of supports fits the care recipient’s situation, followed by collecting required documents and submitting applications to the state or VA. Once approved, the consumer-directed model typically requires provider enrollment, submission of signed care plans or employer forms, and setup of timesheet and payroll pathways that enable weekly payouts. Paid.care’s assistance reduces friction in this chain by offering eligibility checks, coaching, help with paperwork, and weekly payment processing for enrolled caregivers.
The following numbered checklist explains the step-by-step process families generally follow and how Paid.care supports each step.
Check eligibility and program match: Confirm the care recipient’s program eligibility and the most appropriate payment route.
Gather documentation: Collect medical statements, proof of relationship, ID, and care plans required for application.
Submit application and enroll provider: File the program paperwork and enroll the caregiver as an approved provider.
Complete any required training: Fulfill short competency modules or background checks if required by program rules.
Track hours and receive payments: Use a timesheet workflow and payroll setup to get weekly payments.
How to Check Eligibility and Apply for Paid Family Caregiver Programs?
Checking eligibility typically starts with online state portals or program helplines for Medicaid waivers, VA caregiver program offices, and local respite coordinators; these resources provide initial criteria, forms, and timelines. An eligibility check focuses on care recipient enrollment (e.g., Medicaid status), assessed level of need, and whether consumer-directed options allow family members to be paid; timing depends on program backlog but some short-term authorizations can be expedited for emergencies. If families use a facilitation service, that service can run a rapid eligibility review, recommend the fastest program match, and begin preparing documentation immediately. Typical timelines for temporary approvals range from a few days for voucher programs to several weeks for full HCBS waiver enrollments, so early eligibility screening is crucial.
What Documentation Is Required for Caregiver Payment Applications?
Common documentation includes a medical provider statement or care plan that documents the recipient’s needs, proof of the caregiver’s relationship to the recipient, government-issued ID for enrollment and payroll, and signed timesheets or employer/fiscal intermediary forms for payment. Additional requirements may include background checks, signed provider agreements, and brief training certificates where programs mandate competency verification. For temporary or emergency gaps, some programs accept expedited documentation or provisional approvals if an application is filed promptly and core proofs are submitted within a short window. Organizing these documents into a single packet and using checklist-driven coaching reduces mistakes and speeds program reviewers’ ability to approve short-term paid caregiving.
How Are Caregiver Pay Rates and Benefits Structured for Temporary Care?
Caregiver pay for temporary care typically follows three structures—hourly wages, daily rates or stipends, and monthly or lump-sum respite allocations—each determined by the authorizing program and care intensity. Hourly pay is common in consumer-directed Medicaid programs where states set rate ranges based on service type and local wage standards; daily rates or stipends appear in some respite or VA contexts where coverage is episodic. Factors that influence rates include the state’s reimbursement schedule, level of care required (basic assistance vs skilled tasks), caregiver qualifications, and program funding source. Families should compare program rate structures and, where multiple options exist, choose the mechanism that best compensates eligible hours during the temporary gap.
What Are Typical Respite Care Pay Rates for Family Members?
Typical respite pay ranges depend on state reimbursement and service intensity; many consumer-directed programs pay hourly rates aligned with local home-care wages, commonly falling in the low-to-mid tens per hour, while some intensive or specialized respite assignments command higher pay. State-level variation means families in some states may access significantly higher daily rates through specific programs, with reported exceptional examples demonstrating rates that can exceed typical daily thresholds in certain local initiatives. The care intensity—such as medication administration or mobility assistance—often justifies higher pay bands, and certification or demonstrated competence can unlock those elevated rates. Comparing rates across program offers enables families to choose the most financially advantageous short-term arrangement.
How Does State Paid Family Leave Support Caregivers Financially?
State Paid Family Leave (PFL) functions as wage replacement for employed caregivers who take time off to provide or arrange care, and it differs from direct caregiver payments because PFL replaces lost wages for the employee rather than paying the family member delivering care. In situations where a family member is both an employee and a caregiver, PFL may offset income loss while a separate consumer-directed program pays a hired family caregiver; in other scenarios PFL and program payments cannot be combined due to program rules. The interaction depends on state regulations and specific program allowances, so families should verify whether wage replacement and caregiver pay can coexist for the same care episode. Evaluating PFL alongside caregiver pay ensures maximal net benefit during a short-term caregiving gap.
What Support and Resources Does Paid.care Offer for Managing Temporary Care Gaps?
Paid.care provides practical facilitation to navigate program options, check eligibility quickly, and set up payment workflows so families can convert short-term care needs into paid assignments with minimal delay. The company offers caregiver coaching and training—free care coaching and online courses—that help family members meet competency and enrollment requirements faster, and it supports hour tracking and weekly payments through a mobile app. Paid.care’s mobile application performs eligibility checks, enables timesheet submission and approval, and processes weekly payouts, while 24/7 support assists families with setup and eligibility questions. For families in Indiana, Michigan, and Illinois, Paid.care emphasizes competitive pay options, weekly payment cadence, and coaching that reduces onboarding time for temporary caregivers.
Eligibility check: Rapid program matching to identify the fastest payment route for a temporary gap.
Hour tracking and timesheets: In-app timesheets support accurate, auditable records for weekly payouts.
Weekly payments: Regular weekly payouts reduce financial strain during short-term assignments.
Free coaching and online courses: Short training modules prepare caregivers for required tasks and enrollment.
How Does the Paid.care App Facilitate Caregiver Payment and Hour Tracking?
The Paid.care app streamlines the workflow from eligibility check to weekly payment by combining a quick program-match tool, secure timesheet submission, and a managed weekly payout process that reduces administrative overhead for families. Caregivers use the app to log hours, submit them for approval, and receive weekly payments, while the app maintains an audit trail and supports documentation required by state or VA programs. For temporary gaps, the speed of timesheet approval and weekly payout cadence matters most; Paid.care’s system is designed to shorten these timelines and provide transparent tracking for both families and program administrators. The result is a predictable, auditable process that turns short-term caregiving hours into reliable weekly income.
What Training and Coaching Are Available for Short-Term Caregiving?
Paid.care offers free care coaching and online courses tailored to caregivers who must step into temporary or respite roles quickly, focusing on core competencies like medication safety, basic mobility assistance, and emergency response protocols. These modular training options are designed for rapid completion so caregivers can meet program training requirements and confidently perform assigned tasks during short-term coverage. One-to-one coaching supplements courses when caregivers need tailored guidance or assistance completing enrollment paperwork, helping reduce onboarding delays that would otherwise slow approval. By combining targeted training with eligibility support and timesheet tools, these resources help families mobilize capable paid caregivers for temporary needs.
What Are the Tax and Financial Considerations for Paid Family Caregivers?
Receiving pay as a family caregiver creates taxable income considerations, employer or fiscal intermediary reporting responsibilities, and potential interactions with means-tested benefits that families should plan for before accepting paid assignments. The primary mechanism is that paid caregiver earnings are income that may require reporting on a 1099 or payroll form depending on whether a fiscal intermediary treats the caregiver as an employee; recordkeeping of timesheets and payments is essential for accurate tax reporting. Additionally, receiving payments can affect eligibility for other public benefits in some cases, so families should evaluate timing and cumulative income effects when planning short-term caregiving stints. Clear documentation, prudent scheduling of hours, and consultation with a tax professional help maximize net benefit while remaining compliant.
Below are practical strategies families can use to preserve net income and manage reporting risk.
Keep precise records: Maintain timesheets, payment records, and care plan documents to support legitimate income reporting.
Space income when possible: If program rules allow, consider scheduling work to avoid sharp income spikes that impact means-tested benefits.
Use training for higher pay bands: Completing certified training can qualify a caregiver for higher reimbursement brackets in some programs.
How Do Taxes Affect Caregiver Compensation During Temporary Care?
Tax treatment depends on the legal employment relationship: if a fiscal intermediary or employer registers the caregiver as an employee, payroll withholding and employer taxes may apply; otherwise payments might be reported as contractor income. For short-term caregiving, clear timesheet records and written payment agreements help determine correct reporting and avoid misclassification; fiscal intermediaries often handle payroll reporting which simplifies obligations for families. Caregivers should track all received payments and request the appropriate tax forms from the paying entity to ensure compliance. When in doubt, consulting a tax advisor clarifies obligations given program specifics and reduces the risk of retroactive adjustments.
What Strategies Maximize Financial Benefits for Family Caregivers?
Maximizing net income as a paid family caregiver during temporary gaps involves combining allowable benefits, capturing all eligible hours through careful timesheet practices, and using training certifications to access higher reimbursement tiers. Prioritize programs that permit both wage replacement (if you are the employed caregiver) and caregiver pay for another family member when rules allow, and structure hours to reflect actual care delivered while documenting tasks clearly. Completing targeted training can qualify you for higher pay rates in some programs, and consistent recordkeeping reduces delays and payment disputes. These tactics, coupled with eligibility checks and coaching, help families convert temporary care needs into sustainable, compensated arrangements.
For caregivers who want guided help with eligibility, documentation, and weekly payment setup, Paid.care provides eligibility checks, coaching, an app for hour tracking and weekly payouts, and 24/7 support to coordinate fast enrollment—check eligibility and begin the process with the support described above.
FAQs
-
The Rule: Generally, no. Most paid family care programs (especially Medicaid waivers and VA programs) strictly prohibit billing for hours while the recipient is in an institutional setting (hospital, skilled nursing, rehab). Billing for these hours is considered "double dipping" because the facility is already being paid to provide 24/7 care.
The Strategy: Do not log hours for the days the recipient is admitted. However, you may be able to bill for hours worked on the day of admission (before they left) and the day of discharge (once they return), provided you actually delivered care during those specific windows.
-
The Rule: You cannot bill for care you do not provide. If the recipient is staying with other family members who are providing the care unpaid, you cannot log hours during that week.
The Fix: Check if your program allows for "Respite Care" banking. While you won't get paid your standard wages for doing nothing, some agencies allow you to "bank" unused hours to be used later in the month/year, or the recipient might be eligible for a respite budget that hires a temporary substitute, though this doesn't pay you directly.
-
The Rule: It depends heavily on your state and agency. Some states (like California’s IHSS) and unionized home care agencies offer accrued sick pay that you can claim even if you aren't working. However, many independent contractor or "consumer-directed" models do not offer paid vacation or sick leave.
-
The Rule: "Bed-hold" payments (paying to reserve a spot) are common for nursing homes but extremely rare for home-based family caregivers. Agencies generally operate on a "fee-for-service" model: no service, no fee.
The Fix: If you face a long gap (e.g., a month-long hospitalization), you typically have to apply for unemployment benefits or temporary assistance rather than relying on the care program to sustain your income during the break.
-
The Risk: Administrative lag often occurs. If a file is "suspended" due to hospitalization, it doesn't always automatically "unsuspend" the moment the patient returns home.
The Fix: Call your case manager before the care recipient returns home. Confirm that the status code in the payroll system has been switched from "Institutionalized/Suspended" back to "Community/Active." If you skip this step, your first timesheet after the gap will likely be rejected.