Care Plan Documentation: Simple Templates That Help Approvals for Paid Family Caregiver Programs
Care plan documentation is the structured record of a care recipient’s needs, daily activities, clinical assessments, and the tasks a family caregiver performs to meet those needs. Clear, consistent care plans show reviewers why services are necessary, how often support is provided, and the measurable outcomes that justify payment under Medicaid waivers or veteran-directed programs. Many family caregivers struggle with inconsistent logs, vague task descriptions, and missing provider corroboration, which lead to delays or denials for reimbursement. This guide explains what a care plan should contain, step-by-step ADL documentation practices, program types that commonly pay family caregivers, and how to use simple templates to reduce reviewer questions and speed approvals. Practical examples include sample phrasing, EAV-style tables that map tasks to required evidence, and downloadable template guidance to help you populate forms correctly. For family caregivers seeking a practical partner, Paid.care offers app-based tools and coaching to check eligibility, build care plans, and track hours—see the section “How Does Paid.care Support Family Caregivers with Documentation and Payment?” for details on those supports.
Care Plan Documentation for Paid Family Caregiver Programs Clear, consistent care plans show reviewers why services are necessary, how often support is provided, and the measurable outcomes that justify payment under Medicaid waivers or veteran-directed programs. Many family caregivers struggle with inconsistent logs, vague task descriptions, and missing provider corroboration, which lead to delays or denials for reimbursement. Listening to family caregivers: The need to include family caregiver assessment in Medicaid home-and community-based service waiver programs, 2013
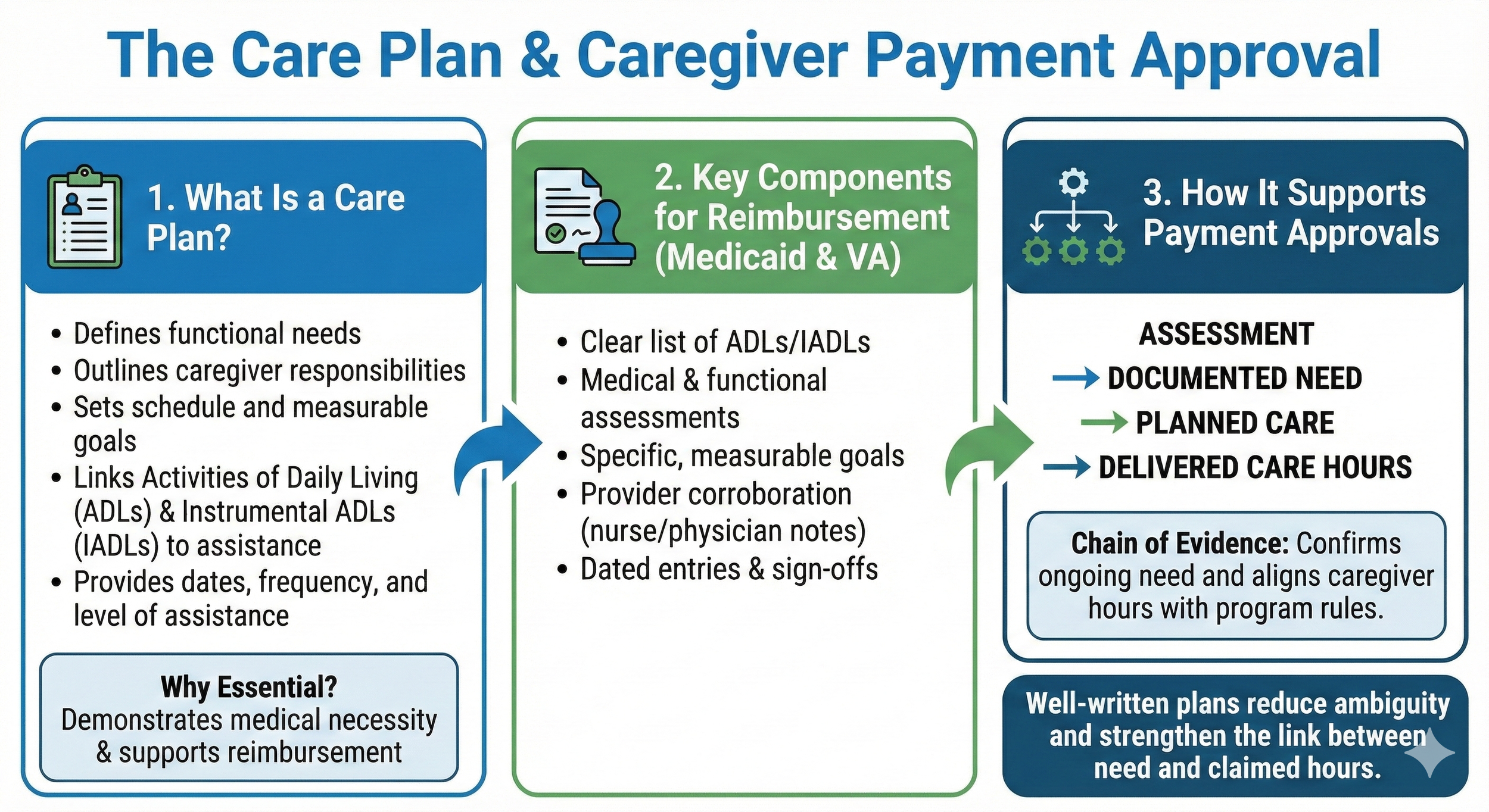
What Is a Care Plan and Why Is It Essential for Family Caregiver Payment?
A care plan is a concise document that defines a care recipient’s functional needs, the caregiver’s responsibilities, and the schedule and measurable goals that demonstrate medical necessity and support reimbursement. This structure links observed Activities of Daily Living (ADLs) and Instrumental ADLs (IADLs) to the specific assistance provided, which helps reviewers determine eligibility and hours payable. Well-written care plans reduce ambiguity by providing dates, frequency, level of assistance, and provider sign-off so payers can match services to program rules. Below we break core components into clear parts and show how documentation supports payment decisions.
What Are the Key Components of a Care Plan for Medicaid and Veteran Programs?
A care plan for reimbursement typically includes a clear list of ADLs/IADLs, medical and functional assessments, specific goals, planned interventions, and signatures from the care recipient or authorized provider. Each component should include dated entries, objective observations, and measurable outcomes so reviewers can confirm ongoing need. Sample phrasing for ADL sections uses active verbs and levels of assistance—e.g., "Assisted with toileting three times daily; requires one-person physical assist for transfers." Provider corroboration such as a nurse assessment or physician note strengthens the link between need and hours claimed. These components set up the evidence reviewers seek when deciding on approval or determining hourly authorizations.
How Does Care Plan Documentation Support Payment Approvals?
Care plan documentation supports approvals by providing a chain of evidence: assessment → documented need → planned care → delivered care hours. Review teams evaluate whether the care described meets program definitions of ADL assistance, whether the frequency matches assessed needs, and whether the caregiver’s hours fit program limits. Strong documentation includes contemporaneous logs, provider sign-offs, and specific descriptions of assistance that map to billing units or hourly caps. The next section shows exactly how to record those ADLs and IADLs so that each entry reads as verifiable evidence rather than informal notes.
How Do You Document Activities of Daily Living for Payment Approval?
Documenting ADLs for payment approval means capturing task, date/time, level of assistance, outcome, and corroborating evidence in a consistent format that reviewers recognize. This method ensures reviewers can cross-reference assessment findings with daily logs and confirm that care meets program criteria for paid support. Best practices include using standardized phrases, including objective observations, and maintaining consistent daily hour totals to avoid apparent discrepancies. The following subsections cover specific fields to capture and how templates convert observations into approvable entries.
What Are Best Practices for ADL and IADL Documentation in Care Plans?
Best practices require recording the date, exact time, specific task, the level of help provided, and an objective observation of the care recipient’s condition. For example: "2025-09-10 07:30 — Assisted with bathing; two-person assist for standing and pivot transfer; skin intact, resident verbalized discomfort 2/10." Use consistent scales (e.g., independent/standby/one-person/ two-person) and avoid vague terms like "helped a little." Keep contemporaneous logs rather than reconstructing events days later, and include provider attestations when assessments change care levels. These habits create audit-ready documentation that directly maps to approval criteria.
Before viewing template examples, consider common documentation elements that reviewers prioritize: ADL task, assistance level, frequency, outcome, and corroboration. A consistent entry format turns daily notes into clear evidence for eligibility determination.
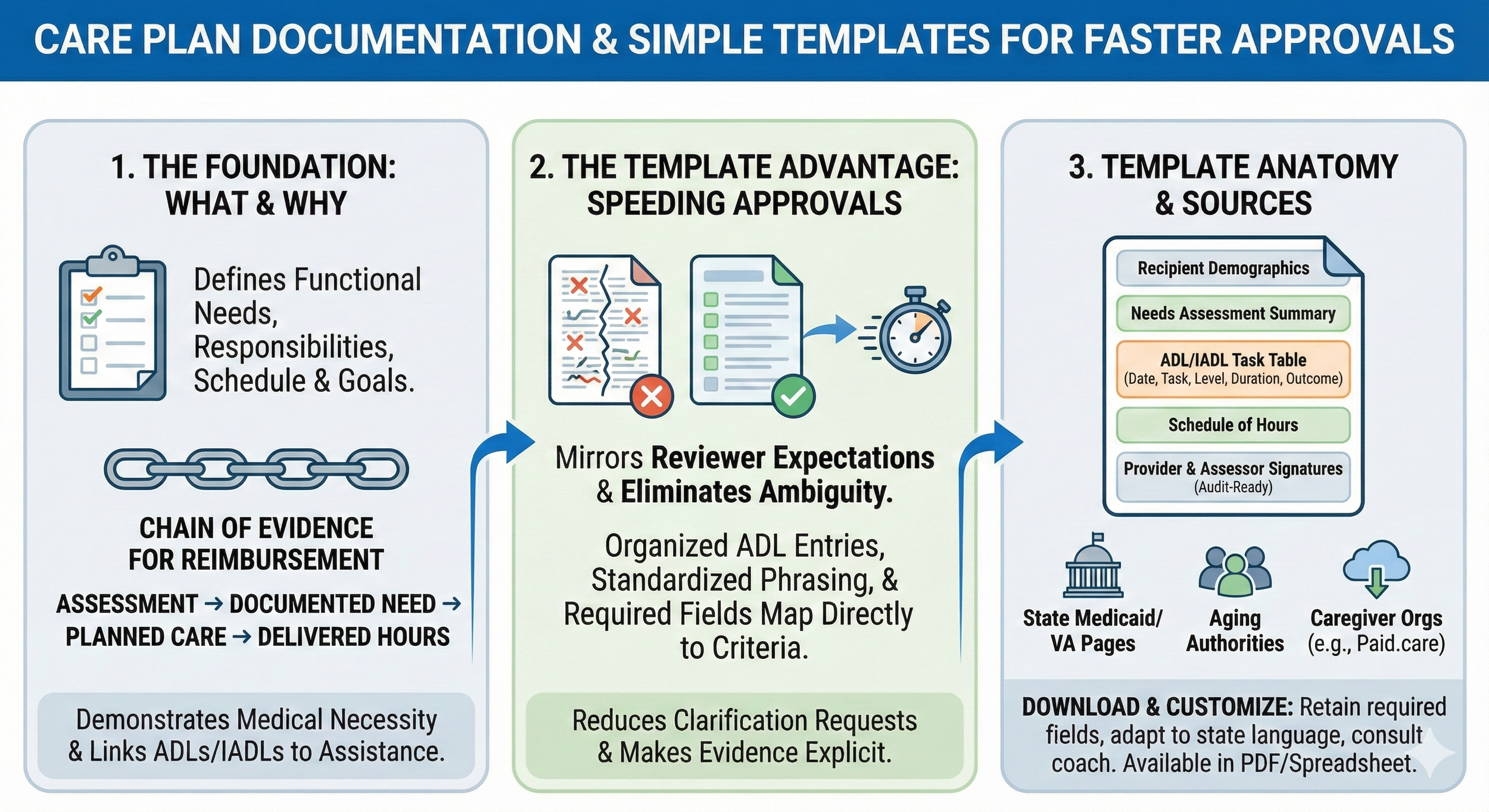
How Can Simple Templates Help Track ADLs for Medicaid and Veteran Caregiver Programs?
Simple templates standardize entries so that each ADL is recorded with the fields reviewers expect, reducing back-and-forth requests for clarification. A compact template typically includes columns for date/time, task, assistance level, duration or units, observations, and sign-off, which makes aggregate hour calculations transparent. Templates can be created in editable formats like spreadsheets or PDF forms that export to PDF for submission, and pre-filled sample entries demonstrate the phrasing reviewers accept. Using templates saves time, enforces consistency across caregivers or shifts, and helps convert daily evidence into the structured packet reviewers need.
Simple templates increase clarity for reviewers by standardizing fields and phrasing.
They reduce reviewer follow-up by including required corroborating information up front.
Templates facilitate accurate hour totals and make appeals easier when needed.
Using templates naturally leads to better audit-readiness and fewer denial triggers, which we illustrate with a documentation table below.
Before the table, note: the next section compares programs that commonly pay family caregivers and what documentation each tends to require.
Which Medicaid and Veteran-Directed Care Programs Pay Family Caregivers?
Medicaid waivers, consumer-directed HCBS programs, and Veteran-Directed Care are program categories that commonly permit payment to family caregivers, each with distinct eligibility rules and documentation expectations. Reviewers look for assessment results, a care plan that maps ADLs to needed services, and contemporaneous logs that verify hours. Payment mechanisms differ: self-directed programs let the care recipient or representative manage budgets and hire family caregivers, while agency models route payments through contracted providers. Understanding these distinctions helps you tailor documentation to each program’s evidentiary standards and increases the likelihood of approval.
What Are the Eligibility Requirements for Medicaid Self-Directed Care in Indiana, Michigan, and Illinois?
Each state applies the general Medicaid waiver principle—functional need demonstrated through assessment and a care plan—but specific forms, terminology, and maximum hours vary by state and program. In general, expect to provide a needs assessment, a care plan with ADL/IADL details, proof of functional limitations, and a schedule of care hours. States often require provider attestations or nurse assessments and may require enrollment paperwork if the caregiver is a paid worker. When preparing submissions, adapt template language to state terms (for example, "self-directed" vs. "consumer-directed") and include the same core evidence elements: assessment, care plan, logs, and provider corroboration.
How Do Veteran Caregiver Payment Programs Work and What Documentation Is Needed?
Veteran-directed programs generally begin with a clinical assessment by VA or affiliated providers, followed by an individualized plan that supports veteran-directed hiring of caregivers, including family members when authorized. Documentation generally requires the VA assessment, a detailed care plan that lists ADLs and the assistance level, and consistent hours logs for billing and oversight. Clinician input and periodic reassessments are often required to maintain program eligibility and justify hours, so include dated clinical notes when functional status changes. Preparing a submission packet with assessment, care plan, logs, and clinician attestations reduces review time and supports continued authorization.
How Can You Create and Use Simple Care Plan Templates to Get Approved Faster?
A template that mirrors reviewer expectations—organized ADL entries, standardized phrasing for assistance levels, and fields for provider corroboration—helps reviewers immediately locate evidence that matches program rules. Templates speed approvals by eliminating ambiguity: when each entry shows who did what, when, how much assistance was given, and what the outcome was, reviewers can quickly confirm medical necessity and hours. The following guidance breaks down required template sections and provides sample language that aligns with approval standards.
What Should a Care Plan Template Include to Meet Approval Standards?
A robust care plan template should contain sections for recipient demographics, comprehensive needs assessment summary, an ADL/IADL task table with assistance levels, measurable goals, planned interventions, a schedule of hours, and signature lines for providers and the responsible party. Each ADL entry should be fillable with date/time, task description, assistance level, duration or units, and objective observations. Sample wording that communicates medical necessity includes phrases like "requires total assist for transfers due to lower extremity weakness" and "requires cueing for medication management due to cognitive impairment." Including a space for the assessor’s signature and date directly beneath the care plan makes the chain of evidence explicit for reviewers.
Required fields ensure each ADL entry maps directly to program review criteria.
Clear sample phrasing reduces reviewer requests for clarification and speeds decisions.
Signature fields and dated assessments make the care plan audit-ready.
Where Can You Download and Customize Care Plan Templates for Family Caregivers?
Trusted template sources include state Medicaid program pages, veteran program guidance, national aging authorities, and organizations that provide caregiver tools and coaching; these sources often offer downloadable, editable templates in PDF or spreadsheet formats. Paid.care also provides downloadable and customizable templates designed to map ADLs and supporting evidence to reviewer expectations, and those templates include sample completed entries that illustrate acceptable phrasing for assessments and logs. When customizing templates, retain required fields, adapt terminology to your state's program language, and add provider signature blocks; consult a care coach or program representative if state-specific forms impose unique fields. Using a vetted template reduces reviewer questions and helps align documentation to approval criteria.
How Does Paid.care Support Family Caregivers with Documentation and Payment?
Paid.care helps family caregivers navigate eligibility checks, build compliant care plans, and track hours using a mobile app plus supportive coaching, making documentation and payment processes easier to manage. The Paid.care App offers eligibility checks, a care plan builder that produces structured documentation, and hour-tracking features that export audit-ready logs for reviewers. Free care coaching and 24/7 support are available to review documentation, suggest phrasing that aligns with program standards, and guide caregivers through application and appeals steps. These services are designed to reduce administrative burden, increase clarity of documentation, and improve the likelihood that authorizations and payments are approved.
How Does the Paid.care App Help Track Care Hours and Build Care Plans?
The Paid.care App streamlines hour logging by providing timestamped entries, task categories linked to ADL/IADL definitions, and exportable summaries that reviewers accept as contemporaneous records. The care plan builder walks users through required fields—assessment summaries, ADL task tables, goals, and signature sections—and outputs a coherent packet that mirrors approver expectations. Exports are formatted to present totals, task descriptions, and daily logs in a clear audit trail, which supports hour reconciliation and appeals if needed. This workflow reduces manual data entry, maintains consistent phrasing across entries, and creates a tidy evidence trail for panels reviewing eligibility.
What Free Care Coaching and Support Does Paid.care Offer to Improve Approval Success?
Paid.care offers free care coaching that includes document review, application guidance, and preparation help for appeals, plus around-the-clock support to answer procedural questions as they arise. Coaches review care plans and logs, recommend wording changes that better align with program review standards, and help caregivers assemble the documentation packet typically required for submission. In practice, coaching can catch missing components—such as incomplete assessment summaries or unsigned provider sections—and advise on corrective steps before submission, reducing denial risk. Accessing coaching is designed to be straightforward and timely, so caregivers can resolve documentation gaps quickly and present a complete evidence packet to reviewers.
What Are Tips and Common Questions About Care Plan Approval for Family Caregiver Payment?
Care plan approval hinges on clear evidence, consistent logs, and corroborating clinical input; small fixes often yield disproportionate improvements in approval likelihood. Presenting a prioritized evidence packet—assessment, care plan, daily/hourly logs, and provider attestations—addresses the most common reviewer needs. The following subsections provide a practical evidence checklist and list common denial reasons with concrete actions to correct them.
How Do You Prove You Are a Paid Family Caregiver for Medicaid or Veteran Programs?
Proving caregiver status requires documentation that demonstrates an employment or service relationship, corroborated hours, and consistent care plan entries tied to assessments. Useful evidence includes a signed care agreement or service plan that names the caregiver, contemporaneous time logs that match assessed hours, payroll or authorization records where applicable, and provider attestations that reference the caregiver’s role and tasks. Organize documents in a packet with a cover page listing included items and dates so reviewers can quickly verify the chain of evidence. Prioritizing these documents in submission reduces processing time and helps reviewers confirm both relationship and service delivery.
Include a signed care agreement or employment authorization when available.
Attach daily/hourly logs that align with the care plan and assessment.
Add provider attestations that reference functional limitations and the caregiver’s role.
When these elements are assembled clearly, reviewers can reconcile hours and authorization more quickly.
What Are Common Reasons Care Plans Get Denied and How Can You Avoid Them?
Common denials stem from vague task descriptions, inconsistent or reconstructed logs, missing provider corroboration, and a lack of measurable goals that demonstrate medical necessity. Avoid these issues by using templates that enforce specific fields, capturing entries contemporaneously, securing provider signatures for assessments, and using standardized phrasing that maps to program definitions of assistance. If a denial occurs, compare reviewer comments with your packet, correct the specific deficiency (e.g., add a dated provider note or clarify assistance level), and resubmit with a brief cover letter explaining the correction. This deny-to-approve approach focuses on targeted fixes that address reviewer concerns efficiently.
Vague descriptions lead to denial; use specific assistance-level language.
Inconsistent hours trigger audits; maintain daily contemporaneous logs.
Missing provider input weakens claims; obtain provider attestations when possible.
Addressing these three areas drastically reduces the most common denial triggers and streamlines appeals when needed.
When preparing documentation, start with a clear needs assessment that lists ADLs and IADLs.
Use templates to standardize daily entries and avoid vague phrases like "helped with personal care."
Secure provider corroboration and signature lines on the care plan and assessment.
These practical steps form an actionable checklist that improves approval odds when implemented consistently. The article has shown what to record, how to phrase entries, which programs require what evidence, and how Paid.care’s tools and coaching can support caregivers in creating audit-ready documentation for submissions.
FAQs
-
A care plan is a written summary of the person’s diagnoses, daily care needs, risks, and the tasks the family caregiver performs. Programs use it as proof that support is medically necessary and ongoing. A clear, organized care plan makes it easier for assessors and caseworkers to see why paid caregiver hours are justified.
-
A basic care plan template usually has these sections:
Client name, date of birth, and diagnoses
Emergency contacts and medical providers
Medications and treatment routines
Daily care needs (bathing, dressing, toileting, feeding, mobility, behavior support, supervision, etc.)
Safety risks (falls, wandering, choking, seizures, self-harm, etc.)
Who provides each task (family caregiver vs. others) and how often
Even a one- or two-page template with these headings can greatly strengthen an application.
-
More specific is better. Instead of “helps with bathing,” write something like “full hands-on assistance with showering 5–6 days per week, including transferring in/out, washing hair, and monitoring for falls.” Include how long each task takes, how often it’s done, and what might happen if the caregiver wasn’t there (for example, falls, missed meds, or unsafe behaviors).
-
Many programs don’t require a provider signature on the actual template, but they do expect the plan to match medical records, diagnoses, and functional assessments. When possible, ask the primary doctor, nurse, or therapist to review the plan or write a brief note that supports the level of care you’re describing. This alignment between documentation and medical evidence helps approvals.
-
Update the care plan anytime there is a major change—new diagnosis, hospitalization, falls, behavior changes, new equipment, or increased supervision needs. For daily logs or timesheets, aim to record tasks in real time or at least once per day. Bringing a recent, updated care plan and a few weeks of daily logs to assessments or appeals can be very persuasive for getting hours approved or increased.
Tell Social Security and any benefits agencies about IHSS income.
Ask how IHSS provider pay will be treated for your specific case.
Many families also work with an advocate or benefits counselor to make sure they keep as much support as possible.